The Achilles tendon was first named in 1963 after the Greek hero Achilles, who was the most important Greek warrior during the siege of Troy. Legend has it that as a baby, Achilles’ mother tried to make him immortal by bathing him in a magical river, holding his heel to keep him from drowning.
This left only the Achilles tendon or Achilles heel vulnerable. It was because of his death from a small wound on his heel that the term Achilles tendon became a synonym for human weakness (Park et al. 2020).
The Achilles tendon, which is about 15 cm long, allows the gastrocnemius and soleus muscles to plantar flex the foot (you lift the toes), and the plantaris and gastrocnemius muscles to flex or bend the knee joint.
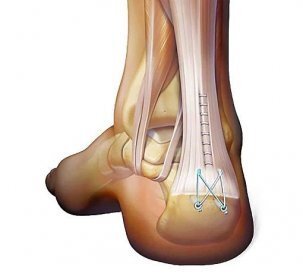
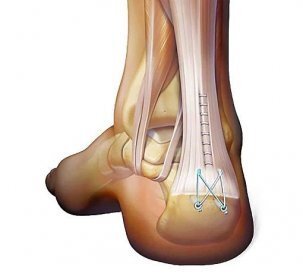
The literature indicates that the rupture of the Achilles tendon occurs in most cases from 2 to 6 cm above the growth point. Any stress on the Achilles tendon that causes it to stretch more than 8 to 10% of its length will result in a complete rupture.
Rupture is most often a spontaneous injury that occurs among active individuals between the ages of 25 and 45. The Achilles tendon ruptures when performing a sporting activity, as there is a sudden push off the ground to run or jump, and this type of injury most often occurs in sports such as basketball, tennis, football, volleyball etc. (Park at el. 2020).
When the tendon breaks, a strong pain is felt, which makes it impossible to rise on the toes or heel, and the gap between the broken ends can be palpated. A hematoma is often visible in the area of the rupture. The foot falls down due to the loss of tone of the triceps surae muscle.
To help check the condition of the rupture of the Achilles tendon, the Simmonds-Thompson test is used, whereby kneading the sword in an injured person lying on his stomach on a soft surface it is determined that the person does not have the strength to perform a plantar flexion movement of the foot. Then the test is positive.
Due to the exporuse of the tendon to insufficient regeneration and thus poor blood circulation just above the growth point, there are not enough nutrients and blood for effective functioning. It is from this point of view that there is a relative lack of good circulation in the lower part of the tendon.
If the rupture is not treated in time, it can re-rupture in another place of the tendon.

After the immediate injury, it is recommended to wear a splint or, in severe cases of pain due to a rupture, to wear a cast. Treatment for an Achilles tendon rupture involves wearing a cast for 6 to 8 weeks, with the ankle in plantar flexion for the first 4 weeks and neutral for the next 2 to 4 weeks. After removal of the cast, the individual independently decides on conservative or operative treatment.
Regarding the surgical approach to Achilles tendon rupture, the risk of re-rupture is reduced to about 5%, the choice of treatment also depends on the type of Achilles tendon rupture. Despite the individual’s decision for operative treatment, the rehabilitation approach after the operative procedure is a guide for restoring strength and endurance.
For the decision to treat with a conservative approach, rehabilitation guided by experts in the field of physiotherapy and kinesiology is the key component that ensures an enabled return to your original sport activities (Holm et al. 2014).
At the Medicofit clinic, we provide good judgment regarding the treatment of Achilles tendon rupture. In general, the surgical approach is not recommended for elderly and/or less active people, as the risk during the operative procedure is overwhelmingly prone to unnecessary side effects
Overloading of the Achilles tendon can occur due to an uncontrolled increase in the amount of training, insufficient regeneration after training, returning to sports too quickly after a long break, inadequate running shoes, poor stabilization of the food and reduced strength and mobility of the shoulder muscles. Rupture of the Achilles tendon has an acute and chronic phase, which means that for the acute phase there is inflammation and the origin of this can be the bursa (bursitis) or the heath of the tendon.
Most often, problems with the Achilles tendon occur at the tendon attachment on the heel or 2 to 6 cm above the attachment.
Due to the reduced tolerance to the loading of the connective structure of the Achilles tendon, all possible problems occur and rest is not sufficient for rehabilitation in the long term.
At the Medicofit clinic, we are aware that gradual loading of the Achilles tendon with exercises is a key part of prospective rehabilitation.
Rehabilitation of a torn Achilles tendon can take up to 12 months and has one of the longest rehabilitation timelines for musculoskeletal injuries.
Since one of the possible complications for Achilles tendon rupture is scarring, exercises to improve range of motion and strength exercises are indicators of success when deciding on conservative treatment.
Physiotherapy role
After removal of the cast or splint, a necessary part of the rehabilitation of the Achilles tendon is the reduction of the stiffness of the musculotendinous structures and the mobilization of the ankle joint. Physiotherapy ensures the healing of collagen fibers, which enables the restoration of the range of motion due to the good elasticity of the structures. In all possible tendon ruptures, at the end of rehabilitation, the connective tissue is reattached.
Physiotherapy also carries out a special application of initial exercises, which depends on how well the tissue is joined without scarring and how well the elasticity and firmness of the Achilles tendon is established.

Although the specifics of the rehabilitation protocol may vary, the focus of physiotherapy and kinesiology rehabilitation is the prevention of re-rupture, where the first 2 months after the removal of the cast or splint is focused on improving muscle strength through exercises, i.e. according to the principle of gradual loading (until pain) and exercises to increase amplitude of movement.
The gradual inclusion of physiotherapy techniques over the next month or during the period of subsidence of the hematoma includes lymphatic drainage, ultrasound therapy, low-energy laser therapy, electrostimulator (ES) therapy, in the Medicofit clinic we use HiTop high-tone electrotherapy and also deep shock wave therapy in the event that other therapies do now treat the injury with sufficient success. We also include TECAR therapy in the initial phase.
Kinesiology takes a leading role in the middle and late stages of rehabilitation of a torn Achilles tendon condition. Three to six months after the rupture of the Achilles tendon, the horizon of accelerated performance of strength exercises and proprioceptive exercises under the supervision of professional personnel from the field of kinesiology begins.
Kinesiology role
In the first month of the exercises, it is recommended to introduce isometric exercises, which are characterized by static holding of various positions while simultaneously resting the muscle attachments. Despite being at rest, a correspondingly large force develops in the muscle.
Of course, when the initial phase of treatment is successfully completed, i.e. during the gradual activation of muscle fibers, the muscle can adapt to the perfect forces, so we continue the training with a directed plan of concentric and eccentric muscle strains of this plyometric approach.
Upon completion of structured rehabilitation under the supervision of experts, it is highly recommended to continue with the exercises that the person previously learned under the supervision of experts in the home environment. By continuing the exercises, possible hyperdorsiflexion of the foot is excluded, as the exercises sufficiently stabilize the entire ankle (Park et al. 2020).
Conclusion
Rehabilitation and healing of the Achilles tendon can take from 6 months to 1 year and the reason for this is the 7.5x lower metabolism of the tendon compared to skeletal muscle.
Likewise, with an incorrect approach to the rehabilitation protocol, individuals may feel pain in the area of the injury for 1 to 2 years after the injury occurred (Holm et al. 2014). A major risk factor for inadequate rehabilitation after Achilles tendon rupture is forms of secondary achillary tendinitis or achilar tendinopathy.
At the Medicofit clinic, we are aware of the possible consequences of ineffective treatment of the rupture of the Achilles tendon, therefore with an approach based on a holistic aspect of diagnostics, physiotherapy and kinesiology, we provide carefully controlled rehabilitation. Damage to the Achilles tendon leads to excellent load bearing capacity!