The terms tennis elbow and golf elbow originate from sports where this type of degenerative condition is common. But definitely don’t let the name fool you – they are not only found in tennis or golf players.
Tennis and golf elbow can be developed by anyone who makes excessive, repetitive movements of the wrist in their daily work. Extremely high loads are not at all necessary for the development of the pathology.
Office workers who keep the wrist in a certain position for long periods of time can also develop tennis elbow. The term tennis elbow refers to a degenerative condition in which the tendons that extend the wrist and fingers and attach to the outside of the elbow are affected.
Golf elbow, on the other hand, is a condition where there is pain in the inner lateral part of the elbow where the tendons that bend the wrist and fingers attach.
Anatomical background of tennis and golf elbow
The ulna is the long bone of the upper arm. It forms the shoulder joint on the upper side and the elbow joint on the lower side, together with the two bones of the forearm, the patella and the humerus.
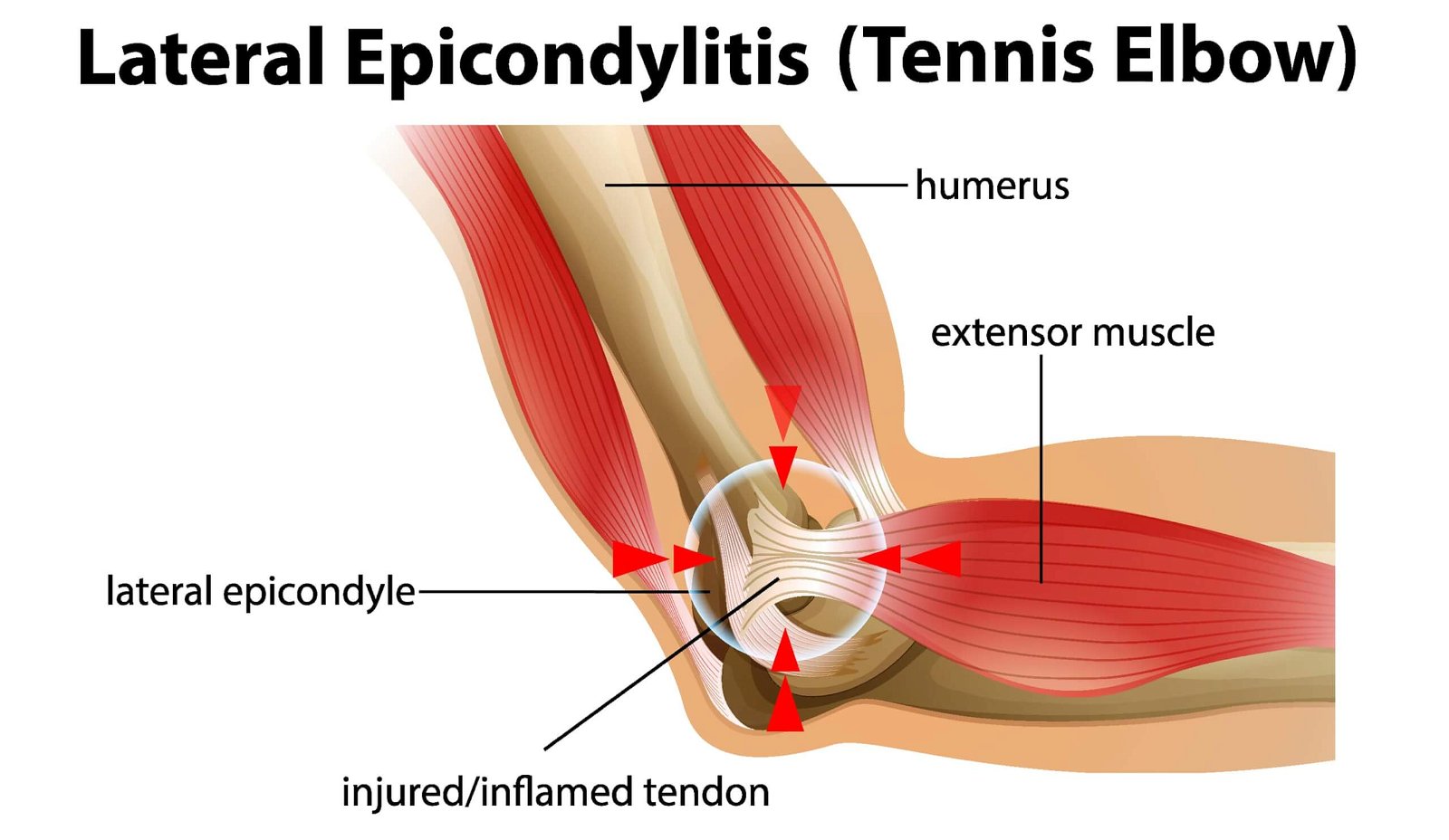
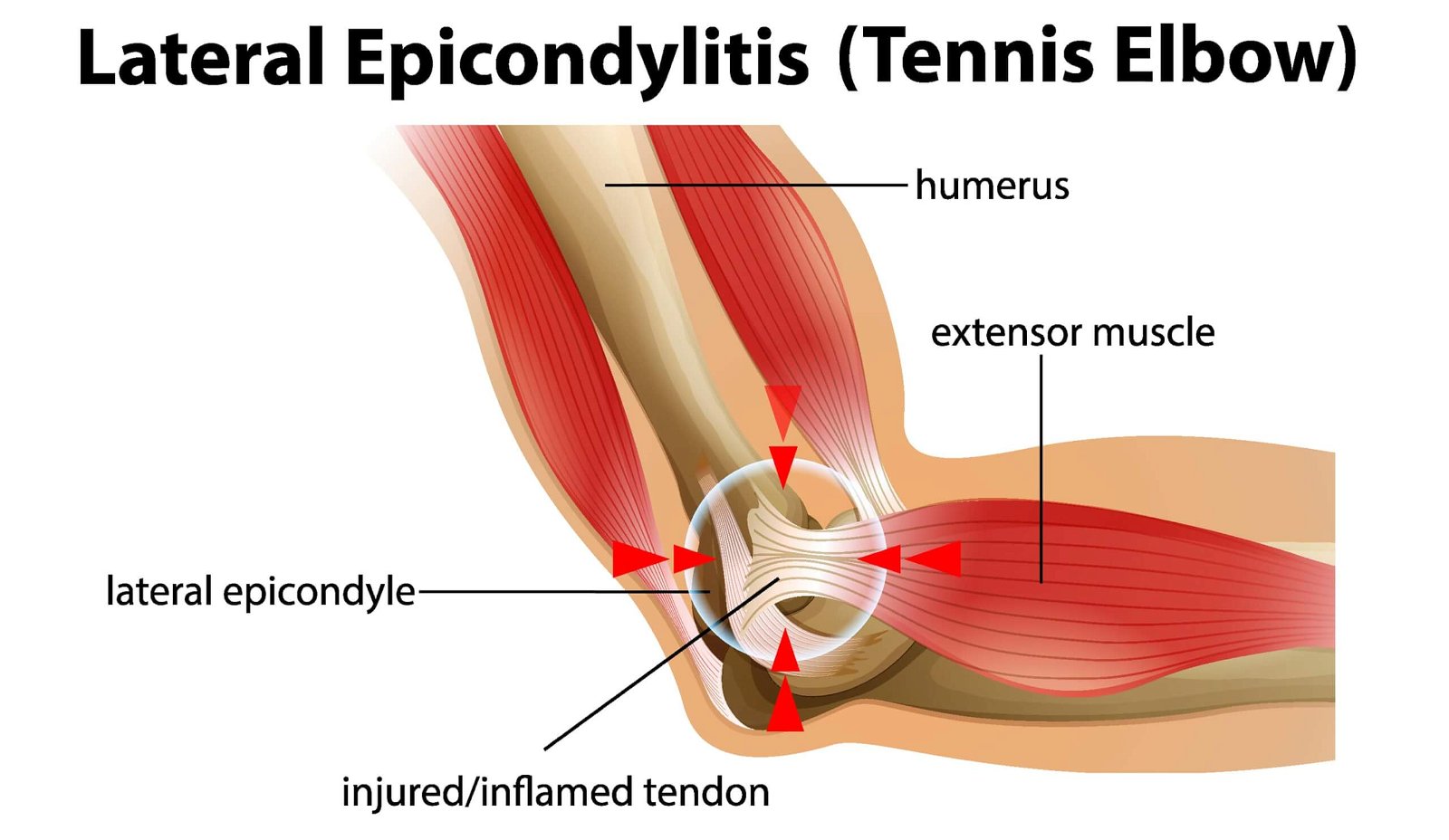
It is important to mention the epicondyles of the humerus. These are the two well-defined knobs on the inner/medial and outer/lateral sides of the lower part of the humerus. The outer epicondyle is attached to the muscles that extend the wrist and fingers, while the inner epicondyle is attached to the muscles that flex the wrist and fingers.
The elbow joint is a hinged joint that allows movement in the direction of flexion and extension. The rotation of the forearm, with the palm of the hand rotated so that it faces the ceiling once and the floor the other time, is made possible by the joint between the patella and the forearm, which also form a joint with each other near the elbow.
The elbow joint is considered to be quite stable. Even in the event of injury, it is more prone to stiffness than instability, compared with, for example, the adjacent shoulder joint, which is also much more unstable because of its great freedom of movement.
The bony system of the elbow joint is surrounded by a rather complex system of ligaments, this is because the individual ligaments are oriented in different directions and the tension of the fibers varies according to the position of the joint, which means that certain fibers are always under tension regardless of position (2).
The elbow joint is also crossed by a large number of muscles involved in flexion and extension of the elbow joint, rotation of the forearm or movement of the wrist. In the diagnosis of tennis elbow, the most sensitive part is just below the lateral epicondyle, i.e. on the outside just below the elbow, where the extensor muscles are located. In the case of golfer’s elbow, the pathology is that of the flexors, which have a common origin at the medial epicondyle (2).
It is important to note that the ulnar and radial nerves also pass through the elbow, the pathology of which must be taken into account when determining a possible differential diagnosis.
Epicondylitis or epicondylalgia?
Epicondylitis is the commonly used name for these two conditions and indicates that there is inflammation of the tendons of the epicondyle. All medical terms ending in -itis define an inflammatory process.
The modern literature on tennis elbow and golfer’s elbow tends to use the term epicondylalgia, because in these conditions inflammation is NOT necessarily always present. It is thought to be a degenerative process, which may be triggered by inflammation in the beginning.
However, inflammation is not usually the main reason for the development of the pathology, and if it is present, it is only in the initial stages of the development of the disease (3). In this article, we will use the term epicondylalgia, or rather tennis elbow or golfer’s elbow.
Tennis and golf elbow involve defenerative changes at the site of the tendons
The pathophysiology of epicondylalgia is multidimensional. It is manifested by changes in tendon cells and their structure, changes in pain signal processing and impairment of both sensory and motor function (1).
This means that excessive loading leads to degenerative changes in the tissue itself – altered cellular activity, disorganisation of collagen strands, repeated microscopic damage, inadequate motor function leading to adhesions, poorer blood flow, slower repair and reduced tissue elasticity (1).
As mentioned above, it can occur on both the outer and inner side of the elbow, with outer epicondylalgia being more common (3).
Tennis elbow is a pain typically just below the elbow on the outer part. It is an overload of the extensor muscles and is a common musculoskeletal disorder in the adult population between 30 and 50 years of age. It affects approximately 1-3% of the adult general population, with no gender differences.
Individuals who smoke, and do a lot of manual work using wrist extensions either in their occupation, household chores, hobbies, or in sports are more prone (1). The condition very rarely occurs in both hands, usually, symptoms occur in the dominant hand and in 20% persist for more than one year (4).
Factors contributing to tennis elbow include handling heavy objects, repetitive movements for more than 2 hours a day, overuse, errors in the athlete’s training process, incorrect technique of movements, ageing, poor circulation, muscular deficits and imbalances.
It is also important to take into account psychological factors such as inattention and thus uncontrolled movement or too intense fist clenching, e.g. of tools in the hand (1). Tennis elbow can also occur as a result of compensatory mechanisms due to poor mobility of adjacent joints (wrist, shoulder, spine) (2).

Clinical diagnostics
Clinically, the tennis elbow is manifested by marked pain, which may be present even at night. At the first clinical examination, the physiotherapist will attempt to reproduce the pain by palpating the affected area, performing a wrist extension against resistance, and squeezing an object in the palm of the hand for diagnostic purposes.
He will examine the entire kinetic chain and assess the adjacent joints for mobility and muscle activity. The treatment of tennis elbow can be lengthy and complex, and good management requires a good evaluation of functional activities, both motor and sensory. In the case of the athlete, it is essential to assess the status in sport-specific activities (1).
Get professional help at MedicoFit
Four guidelines guide therapists in deciding on specific treatments and patients in participating in each rehabilitation process. What are the benefits of the chosen therapy, what are the risks, what are the alternatives and if any, and what are the consequences of doing nothing. There is no one-size-fits-all prescription for tennis/golf elbow rehabilitation.
It requires planning, checking and ongoing adjustment according to each individual’s response to the chosen therapy, and their current lifestyle. Patient participation in the rehabilitation process is essential – and this is where Medicofit excells at.

It is important to adapt the working environment to the best of your ability. This means trying to minimize activities that trigger pain. Try to ensure that the wrist is as neutral as possible with various ergonomic aids, and that there is enough rest and recovery time (1).
Maintain the level of movement at the highest level possible wherever possible and do not exceed the pain level of 3/10.
Bear in mind that the process can be lengthy, and as a first step – seek professional help.
- Coombes BK, Bisset L, Vicenzino B. Management of Lateral Elbow Tendinopathy: One Size Does Not Fit All., 2015. J Orthop Sports Phys Ther. 45(11):938-49.
- Physiopedia. Lateral Epicondylitis. Avaliable at: https://www.physio-pedia.com/Lateral_Epicondylitis#cite_ref-:4_6-1 [10.4.2022]
- Reece, C.L. & Susmarski, A., 2022. Medial Epicondylitis. Avaliable at: https://www.ncbi.nlm.nih.gov/books/NBK557869/ [10.4.2022]
- Walz, D.M., Newman, J.S., Konin, G.P. & Ross, G., 2010. Epicondylitis: Pathogenesis, Imaging, and Treatment, RadioGraphics, 30(1): 167 – 184. Level of Evidence: 2C
How is the rehabilitation of tennis and golf elbow?
The course of treatment is always tailored to the individual characteristics. For those at low risk of deterioration, we try a “wait and see” approach. In English, this would be translated as “wait and see”. The body has the capacity to heal itself and sometimes it just needs rest and time.
Individuals are advised to reduce or limit pain-inducing activities, to dose themselves with pain relief therapy in the form of painkillers, and apply hot or cold compresses according to their own needs. After 6-12 weeks, a reassessment of the condition is necessary.
If the condition has not improved significantly, multimodal physiotherapy is tried from the outset in all those at medium or high risk of a poor prognosis. The majority of patients are in this group. This includes all those who handle heavy loads on a daily basis or have a lot of repetitive hand movements that cause them discomfort. Physiotherapy is also started in all those who have an associated pathological condition in the elbow or adjacent joints or significant neuromuscular impairment (1).
Physiotherapy phase
Physiotherapy treatment includes ergonomic or sports-specific advice. If necessary, analgesics, and cooling/warming of the affected area are advised. Various kinesiotaping techniques are also used and splints may be recommended to help control wrist position. We advise electrophysical agents as pain relief therapy, and we also perform manual therapy on the elbow area, where we use various techniques to try to help with facilitation of proper tissue gliding.
Kinesiotherapy phase
Kinesiotherapy is a very important part of our treatment plan, where we try to correct any weakness or muscle imbalance by using a progressive model of muscle strength training, teaching motor control and performing exercises to build strength in the whole upper limb.
In athletes, especially racquet handlers, we do not forget plyometric training as we want to improve elastic load tolerance during explosive muscle contraction. During exercise, we tolerate a pain level of up to 3/10, which should not persist into the next morning. If there is no significant improvement after 8-12 weeks of regular and consistent therapy, we advise diagnostic imaging (ultrasound or MRI) to confirm the diagnosis or to investigate the differential diagnosis and to modify the treatment plan.
It is possible that there is a tendon rupture, ligament or nerve injury, possible musculoskeletal pathology, etc. If the imaging confirms epicondylalgia, serious modification of work or sports activities is needed.
Additional pharmacotherapy should be discussed, exercise should be resumed and specialist/chiropractic referral should be obtained (1).