Intense pain in the buttocks that spreads down the legs or the leg is often associated with problems originating from the spine, e.g. due to disc herniation or effusions of the intervertebral discs.
Piriformis syndrome is a condition that is difficult to distinguish from sciatica, which is caused by compression of the nerve pathways at the level of the spine.

What is piriformis syndrome?
Piriformis syndrome is difficult to diagnose, as it often has the same symptomatic picture as sciatica, which originates from problems with the spine. Sciatica is the result of dysfunction of the lumbar spine, where the nerve is compressed by disc herniation, spinal stenosis or arthrosis, for example.
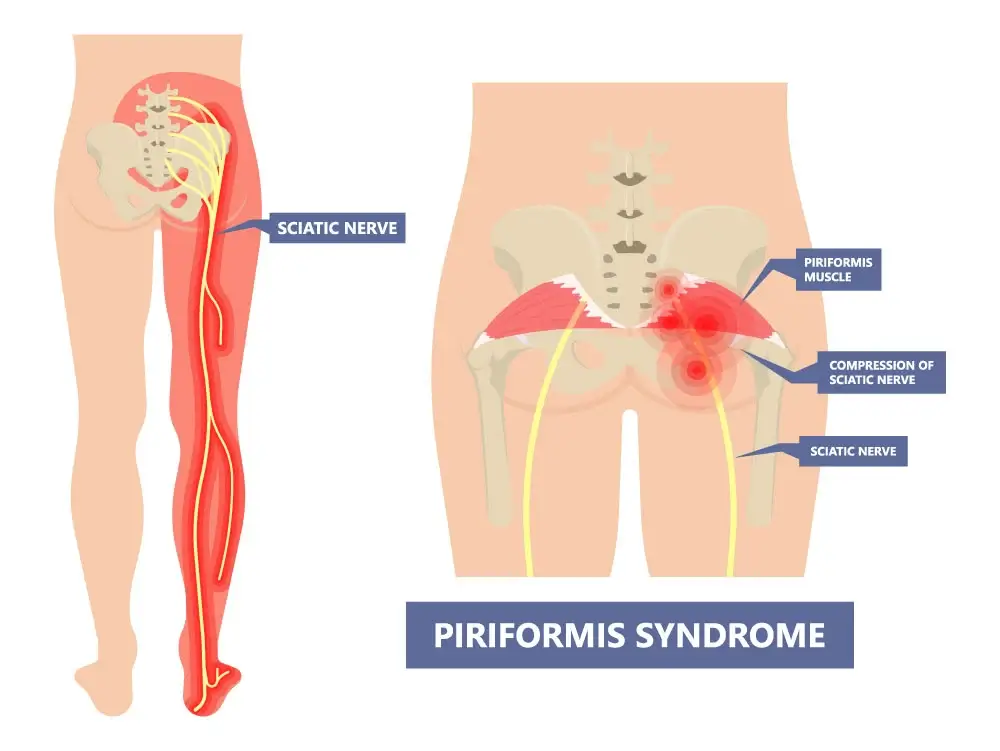
Piriformis syndrome, however, occurs when the deep buttock piriformis muscle, due to excessive tension, pinches the sciatic nerve, which lies directly below it. Piriformis syndrome is thus compression of the sciatic nerve, caused by the piriformis muscle.
It is pain that radiates from the buttocks and spreads down the back of the thigh with possible distal symptoms to the foot. In a strong acute form, Piriformis syndrome can also radiate to the area of the lumbar spine, but it is of greatest intensity in the area of the hip.
Understanding the anatomy and function of the piriformis muscle and sciatic nerve is key to distinguishing between discogenic sciatica and piriformis syndrome.
How does the piriformis muscle work?
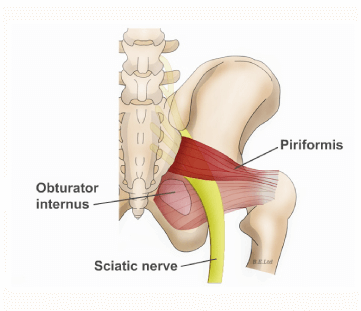
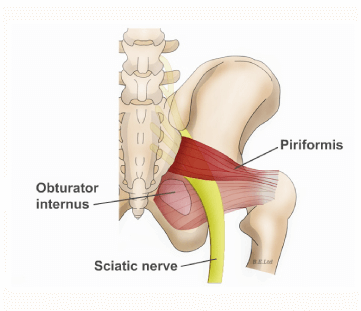
The piriformis muscle or the pear-shaped muscle is a muscle of the deep gluteal musculature and lies directly under the gluteus maximus muscle or gluteus maximus. The deep gluteal muscles are m. Piriformis, m. Obturator internus, m. Quadratus Femoris and m.Gemellus superior and m. Gemellus inferior.
The piriformis muscle is the most superficial muscle of the deep gluteal muscle group and represents a sensitive anatomical area, it passes through the large sciatic foramen in the pelvis, and the sciatic nerve enters directly below it.
Did you know that the sciatic nerve is only 1.5-3 cm away from the piriformis muscle on average, but in certain anatomical variations it is less than 0.9 cm? ,
The piriformis is a deep lateral stabilizer of the hip joint, it primarily performs external rotation of the hip, but also assists in abduction, extension, internal rotation and flexion of the hip. The function of the piriformis muscle is to stabilize the pelvis during rotational loads in synergy with the other deep gluteal muscles.
Pseudoscience often misinterprets that it is necessary to strengthen the piriformis muscle for better stabilization of the pelvis, e.g. in connection with running loads. The piriformis muscle is in fact a ‘reserve fuel’, the primary stabilization and carrying of larger loads is performed by the large muscle groups of the hip m. Gluteus Maximus and m. Gluteus Medius. As part of the rehabilitation of piriformis syndrome, it is primarily necessary to adequately strengthen the main muscle groups of the hip and to treat the piriformis muscle against pain and inflammation.

Causes of piriformis syndrome
The most common cause of piriformis syndrome is overloading the piriformis muscle, which occurs as a result of poor muscle function of the large gluteal muscles m. Gluteus maximus and m. Gluteus medius. Articles often state that intense running can be one of the causes, but when running, it is actually a matter of poorer local muscle endurance of the large gluteal muscle groups, which causes excessive activation of the piriformis muscle, which primarily performs the function of a stabilizer.
When m. Gluteus maximus and m. Gluteus medius ‘fails’ and their role is taken over by the piriformis, which becomes shortened and stiffened due to overload.
The sports activity that is most directly related to piriformis syndrome is cycling due to long-term direct pressure on the piriformis area and intense repetitive loading.
Overloading of the piriformis muscle can also occur directly due to increased long-term pressure on the piriformis muscle in the form of long eccentric loads or direct pressure, e.g. when sitting.
Piriformis syndrome can also be caused by prolonged walking in combination with inadequate hip mechanics due to shortened hip muscles.
Individuals with an anatomic variation where the distance between the piriformis muscle and the sciatic nerve is less than 1.5 cm are at greater risk. Anatomical variations mean that the sciatic nerve lies in different relationship to the piriformis muscle, in fact in can run above or below the piriformis muscle at different distances from it.
Book an appointment for piriformis rehabilitation!
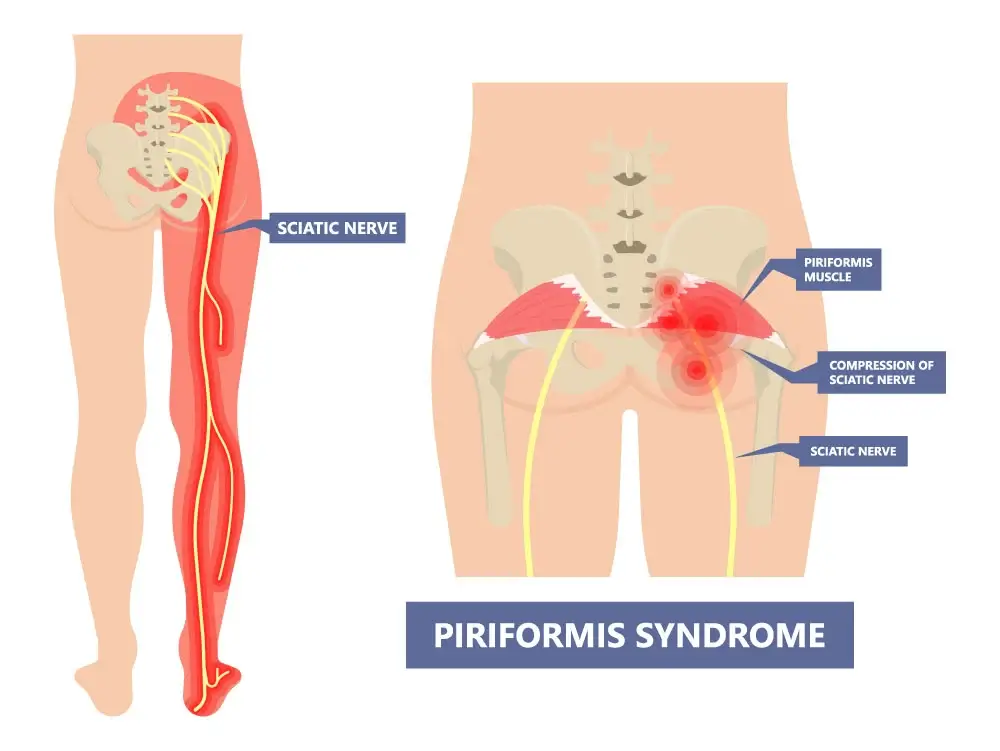
Piriformis syndrome is characterized by severe pain in the buttock area, which occurs more often on one side than on both sides, and the pain can radiate down the leg to the foot. Distal pain in piriformis syndrome runs down the back of the thigh.
One of the characteristics is that direct pressure on the piriformis muscle worsens the pain symptoms, especially sitting on hard surfaces in unbearable. It is also aggravated by increased activation of the deep gluteal muscles, e.g. a long-term condition or intensive exercise for the lower limbs, cycling and in the acute phase, even walking.
A severe acute state of piriformis syndrome is also characterized by limited mobility in the hip, tingling and sensory numbness in the buttock area.
Bilateral asymmetry in the strength of the hip abduction and external rotation will also be characteristic, the affected side will be painfully limited in the muscle activation of the gluteal muscles.
How do we distinguish between sciatica and piriformis syndrome?
Piriformis syndrome is often difficult to distinguish from sciatica, which is caused by pathologies of the spine or discogenic pain. It is important that the physiotherapist performs differential clinical testing and gradually eliminates all possible causes of sciatica symptoms at the level of the spine. In practice, the basic understanding of the clinical picture of sciatica and piriformis syndrome is often only superficial. Piriformis syndrome is not accompanied by back pain or if this is only present when the patient is in highly stimulated state, patients can easily determine that it is the origin of the pain in the hip area.
However, we must be aware that the mere absence of pain in the lower back is not enough for the diagnosis of piriformis syndrome, as sciatica can also manifest itself in various forms, e.g. with the complete absence of low back pain or the lumbar spine, which can be present only in the gluteal region or only distally in the area of the ankle or throughout the lower limb without radiation to the lumbar spine.
At the Medicofit clinic, when piriformis syndrome is suspected, we often test direct palpation of the piriformis area and at the same time take a detailed history of pain in the lower back, hips and lower limbs. A detailed medical history by a physiotherapist when piriformis syndrome is suspected plays a key role, as patients with discogenic pain or problems cause by sciatica described problems with back pain in the past.
We must be aware that in rare cases of spinal entrapment of the sciatic nerve, it can also be a complete absence of back pain in the past or for sciatica for asymptomatic spine.
It is important that the clinical diagnosis in carried out by a suitably qualified physiotherapist, who will be accurate in the test of direct palpation of the piriformis. We know from clinical practice that in the case of piriformis syndrome, direct palpation of the muscle will be sensitive, and by increasing the pressure we will achieve greater irritation of the condition.
It is important that the physiotherapist performs all clinical tests for neurological entrapment at the level of the lumbar spine and also performs a ‘load test’ of the spine for the appropriate differential diagnosis of piriformis syndrome.
How does physiotherapy work for piriformis syndrome?
In the initial acute phase of the irritated piriformis muscle, we perform neurodynamic exercises for the sciatic nerve and make sure that we do not increase the pressure on the nerve with treatment methods. Aggressive trigger point therapy is contraindicated in the acute phase, and the same applies to forced stretching, as botch can worsen the tense state. We perform TECAR therapy and laser therapy to reduce pain or the excitability of the state. When the symptoms improve, we start with manual techniques and exercises to obtain optimal mobility of the hip joint.
The key to piriformis syndrome is the building of adequate load-bearing capacity of the hip in the form of increased endurance in the strength of muscle groups m. Gluteus maximum and m. Gluteus medius. It is also important that the movement patterns at the end of the rehabilitation are appropriate with the absence of comprehensive movements or muscle deficits.
For athletes, we perform full loading of the hip in a closed kinetic chain and sport-specific testing.
How long does physiotherapy for piriformis syndrome take?
Comprehensive physiotherapy treatment lasts between 4-6 weeks to achieve all rehabilitation goals. Each patient must understand that eliminating the pain of piriformis syndrome is only the first phase of treatment, and the restoration of full movement function and optimal functioning of movement patterns is the norm for completing rehabilitation in the second phase of treatment. In cases where it is a chronic condition or a highly agitated condition present for a long time, physiotherapy can last up to 10 weeks.
Book an appointment for piriformis rehabilitation!
Did you know that stretching the piriformis muscle can often worsen piriformis syndrome and pain?
Few areas of pain rehabilitation and physical therapy contain the dimensions of pseudoscience that occurs in relation to the conditions of piriformis syndrome, sciatica and low back pain. Piriformis syndrome is a condition that is often caused in combination with gluteal muscle dysfunction. The most common advice for piriformis syndrome has become myofascial relaxation in the form of assistance with a massage roller or ball (foam rolling) and piriformis stretching, which are often exercises that increase direct pressure on the piriformis. These are quick solutions that are not aimed at holistic treatment and can lead to chronic piriformis syndrome.
Piriformis syndrome is a condition that has a difficult way of establishing a diagnosis, which must be differentiated by clinical tests, a detailed history, palpation tests and muscle strength tests.
You may have piriformis syndrome when you are dealing with chronic pain in the buttock of severe acute pain in the back or outside of the hip that radiates down one or both legs. At that time, it is a compression of the sciatic nerve, which is the longest and thickest nerve in our body, and it animates our lower limbs. Sciatic nerve entrapment can be discogenic at the spinal level or myofascial caused by the piriformis muscle.