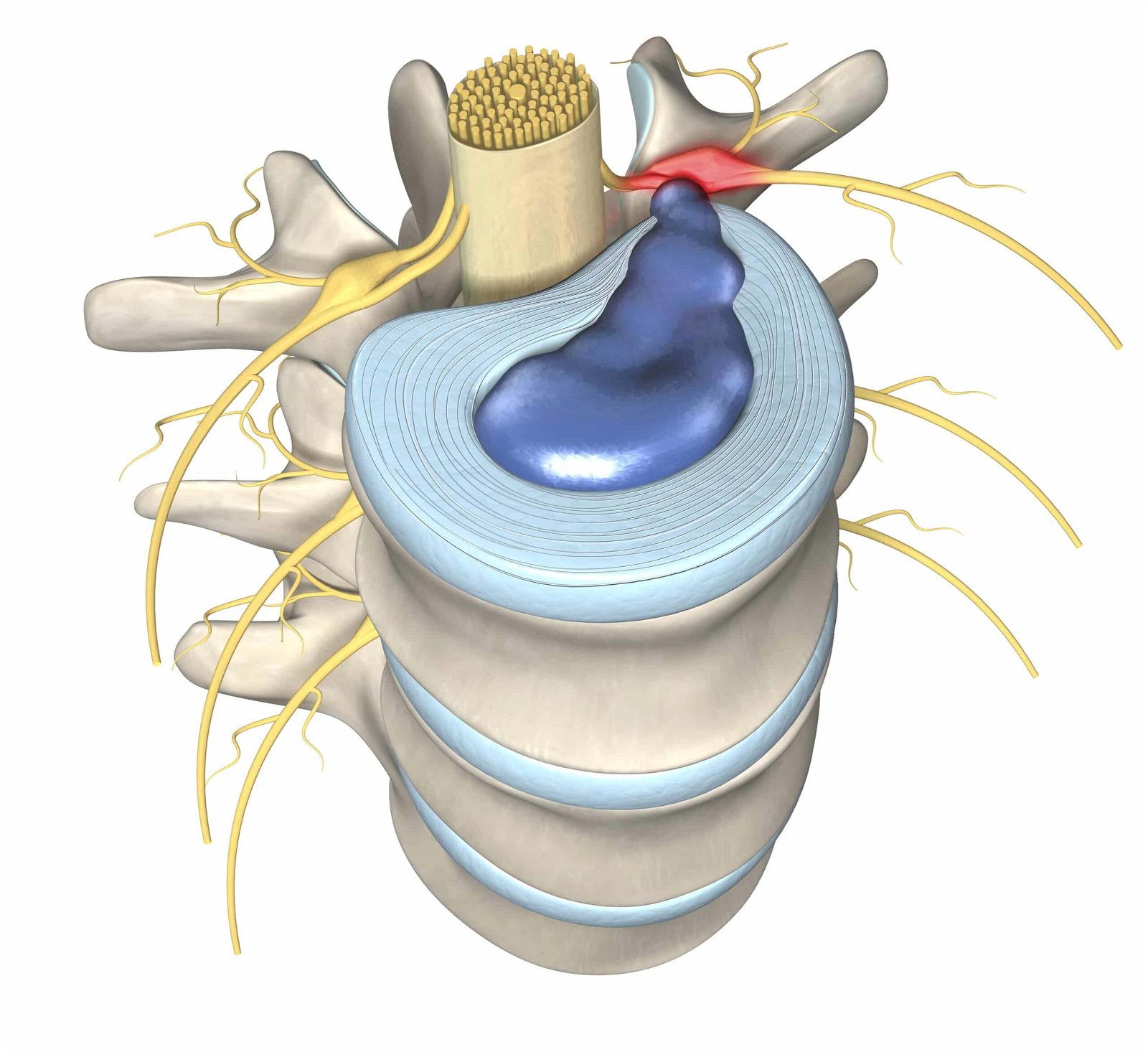
Facet joints are small joints of the spine between the vertebrae, located posterolaterally on the vertebral arches, with the facets of the upper and lower vertebrae in each pair contacting each other.
Each vertebra of the spine has a total of four facets, two on each side, below and above.
The fibres of the multifidus muscle group, which play an important role in stabilising the spine, attach to the small facet joints. The synovial membrane of the facet joints is also attributed with an important proprioceptive function due to the high number of mechanoreceptors present.
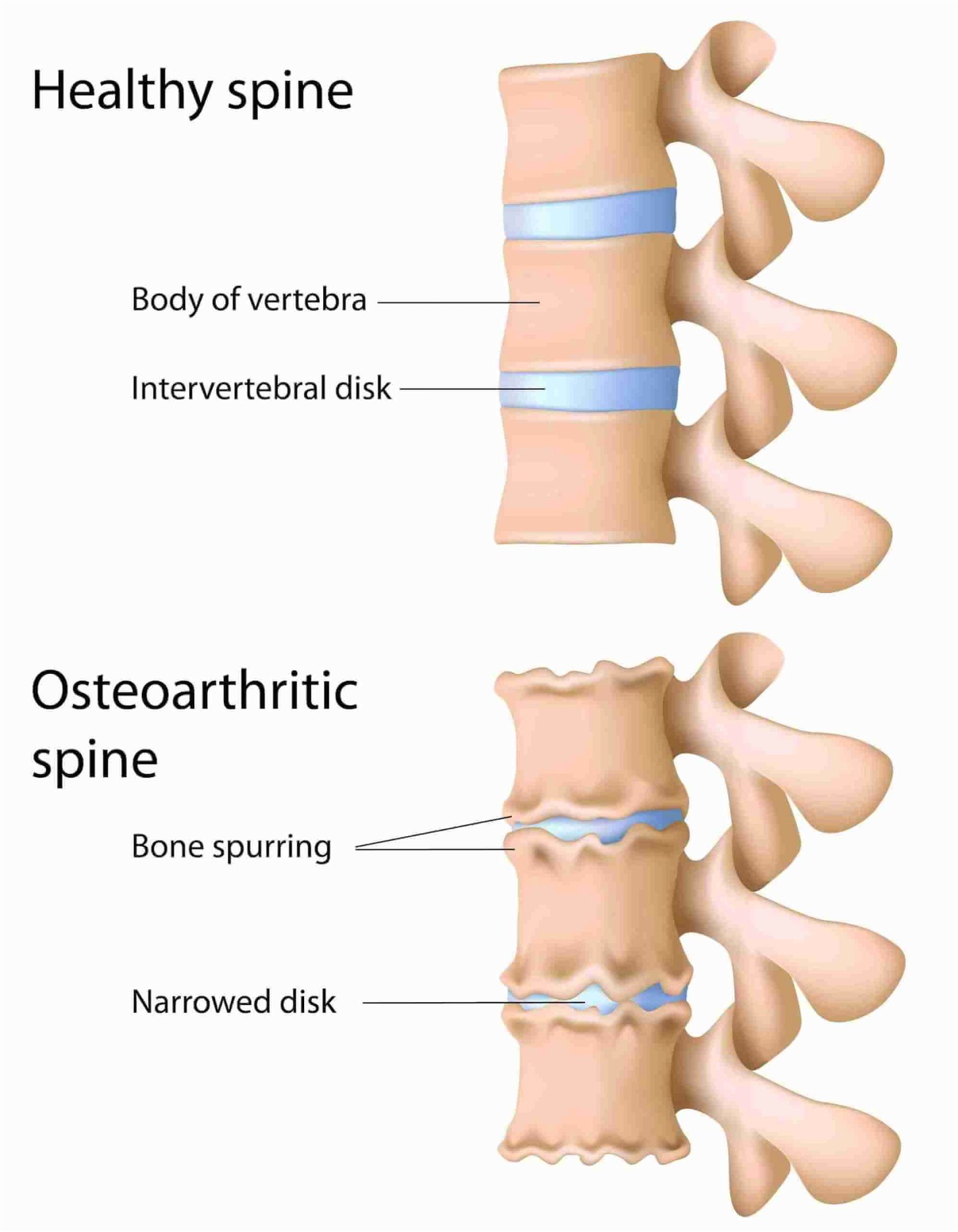
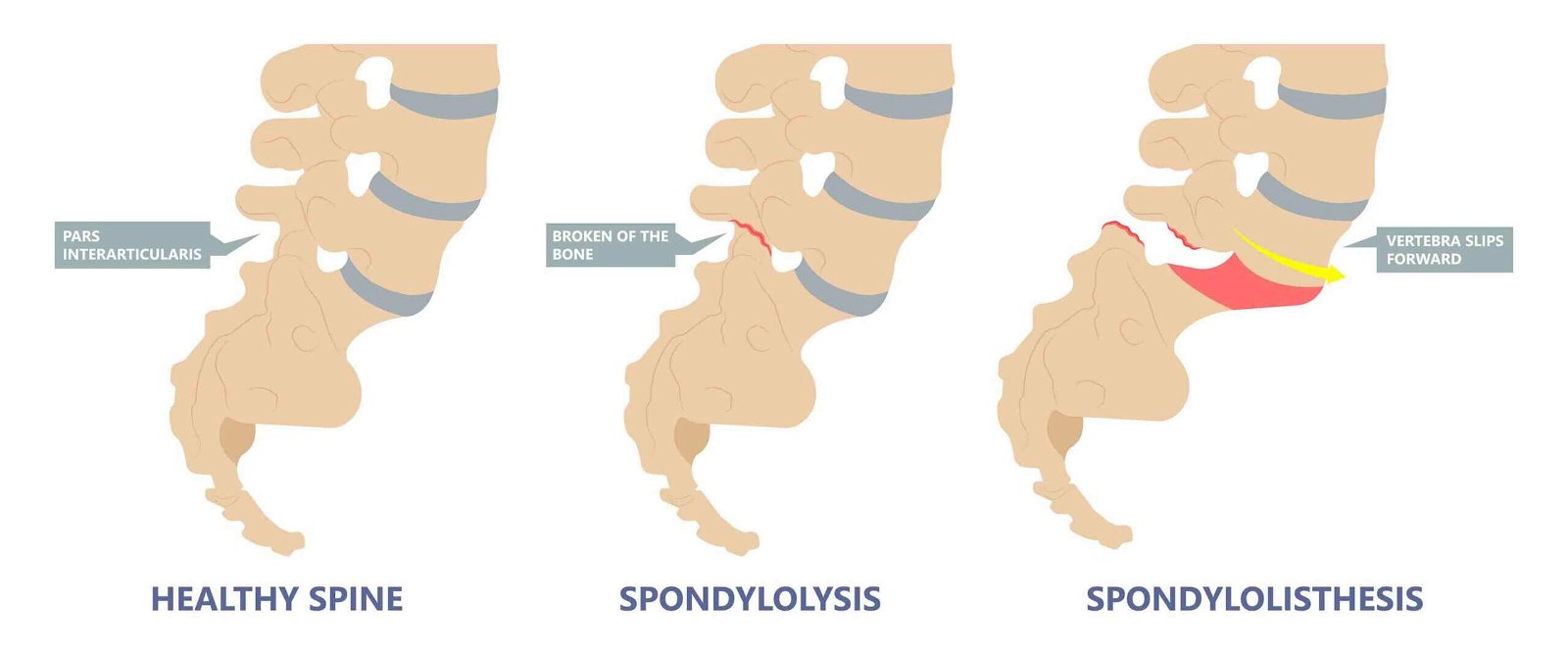
Before starting treatment for pain originating from injury or wear and tear of the facet joints, an accurate diagnosis is necessary, as several different degenerative spinal conditions cause similar symptoms.
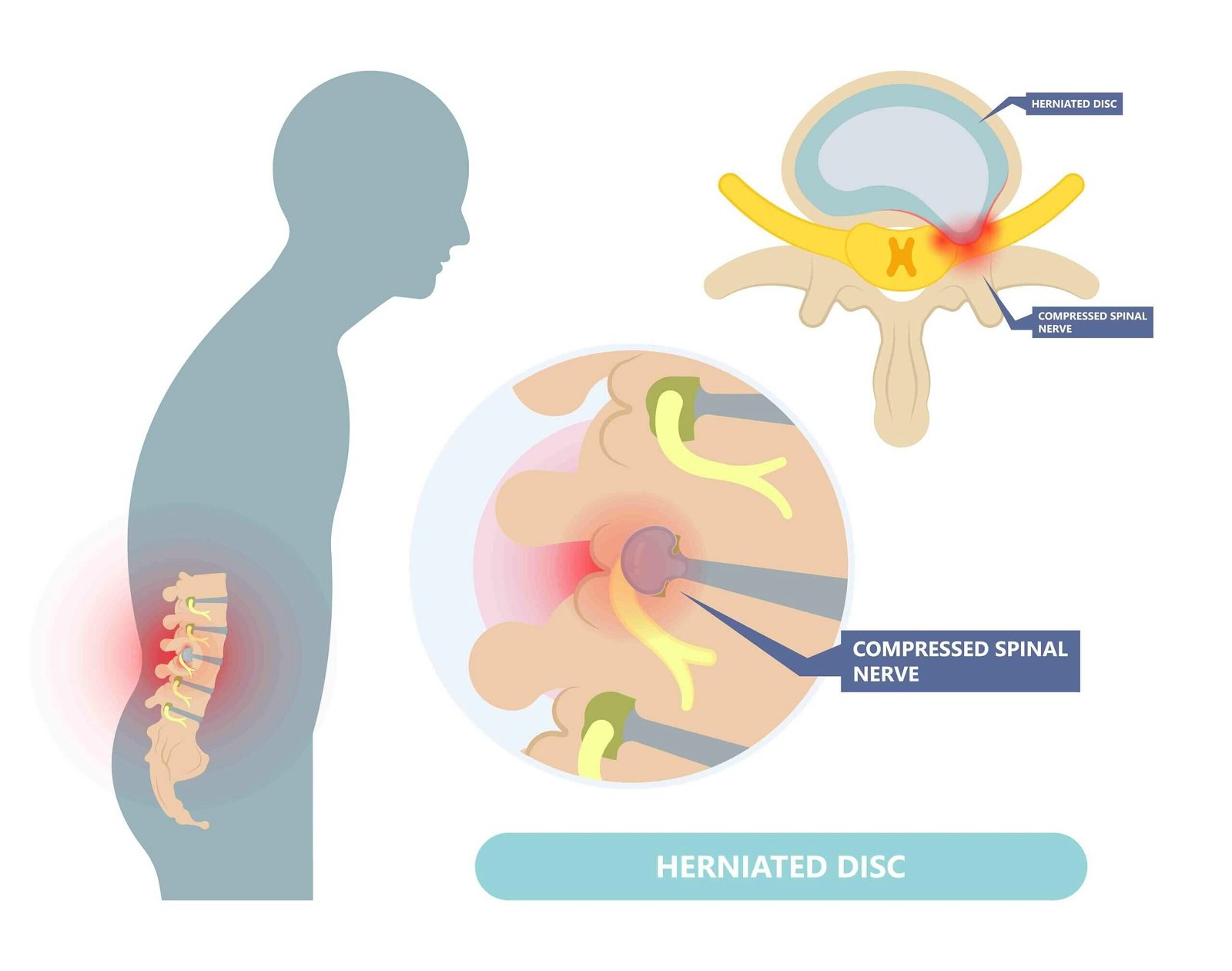
Pain originating from facet joint degeneration becomes more intense with specific movements such as turning the torso or head, while in the case of a herniated disc, symptoms are aggravated primarily by sitting, which is often worst in the morning.
In the case of a herniated disc, the pain occurs on the opposite side of the protrusion, while in the case of a facet joint injury, the pain symptoms occur on the same side. When a facet joint of the cervical or thoracic spine is injured, neurological symptoms do not radiate to the arms, as is often the case with a herniated disc at the same level.
Pain resulting from facet joint degeneration or injury is usually present in the immediate vicinity of the damaged tissue right next to the spine; in the case of cervical facets, the pain may radiate to the back of the head, and in the case of thoracic facet injuries, the pain is often between the shoulder blades.
The pain is usually burning or stabbing with quick and jerky movements of the cervical or thoracic spine, and often becomes dull and more difficult to define with prolonged postures.
Treatment of symptoms resulting from wear and tear of the facet joints is carried out after initial MRI and/or X-ray diagnostics and after clinical tests have been performed.
Conservative treatment is aimed at slowing down the degeneration of bone and cartilage surfaces and stopping the thinning of the intervertebral discs.
It is important to perform appropriate instrumental physiotherapy to alleviate acute symptoms and training to strengthen the deep stabilising muscles of the spine and maintain mobility in key affected segments.
The conservative programme should be implemented intensively for three to six months, then it should move into the maintenance phase or degeneration management, which should take place in the long term as a less intensive programme, e.g. twice per week.
In the initial stages of spondylosis, conservative treatment is recommended, which is tailored depending on the level of spondylosis and the symptoms caused.
The training part of conservative treatment of spondylosis is aimed at:
strengthening stabiliser muscles,
maintaining mobility,
preventing muscle atrophy.
In the early stages of spondylosis, conservative therapeutic techniques are highly effective in slowing the spread of spondylosis and reducing acute symptoms.
Surgical treatment of spondylosis is performed when spondylosis causes dysfunction of internal organs and vital functions, severe compression of the spinal canal, or major neurological disorders in the extremities.