Did you know that meniscal injury is the leading reason for arthroscopic knee surgery?
In the USA, they perform e.g. 400,000 meniscal surgeries every year. You probably didn’t know that meniscal injuries can be asymptomatic, i.e. not painful, but still dangerous if not treated correctly. But you probably didn’t know that active physiotherapy is a mandatory method of treatment for all types of meniscus injuries and is a priority before performing surgical treatment for almost ¾ of all meniscal injuries.
We will also give you a basic medical explanation of the types of meniscus injuries with the relevant terminology, because we believe in transparency, so we want you to have a good understanding of your injury. At the Medicofit clinic, we say that the patient’s understanding of his condition is the key to successful rehabilitation, because only then will the patient be able to make the right decision regarding the type of treatment in the midst of all the information and expert opinions.
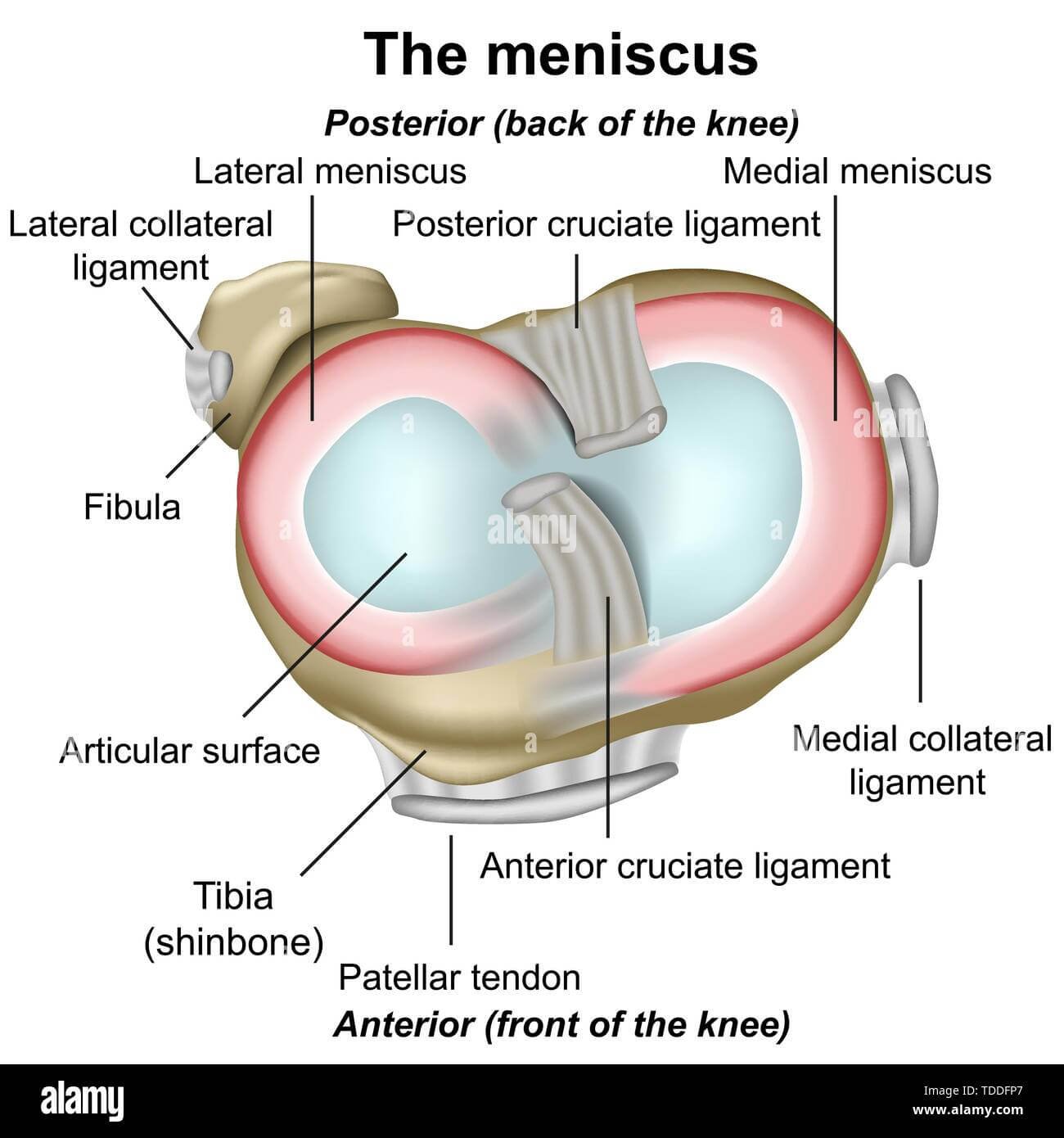
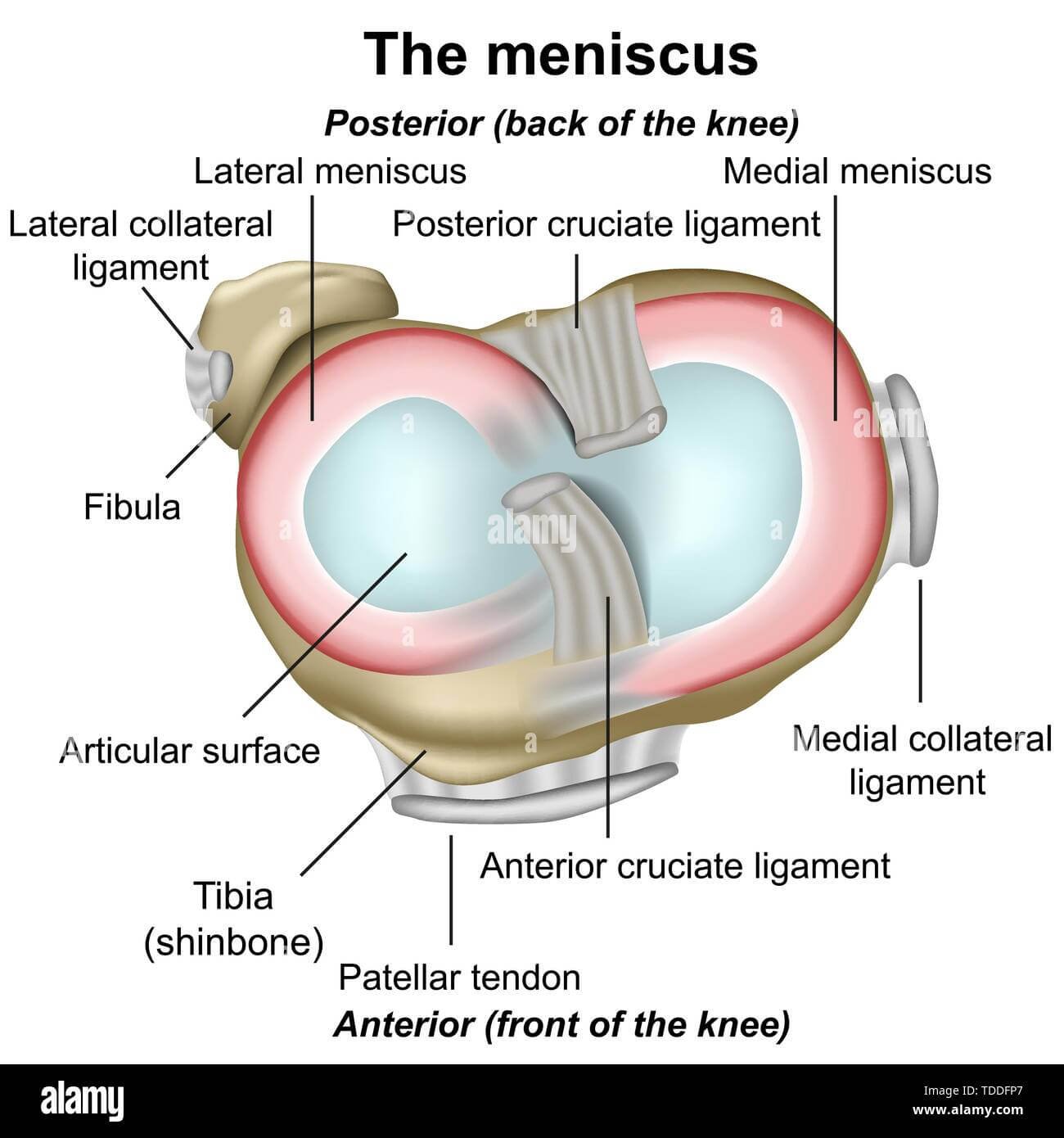
The meniscus is a wedge-shaped connective-cartilaginous structure in the knee joint. Each knee has two menisci, the medial meniscus of the inside of the knee and the lateral meniscus on the outside of the knee. The function of the meniscus is often only superficially understood in practice, so below we give you an explanation of the function of the meniscus in a way that is easy to understand.

How does the meniscus work?
The meniscus is primarily a knee joint strengthener, it can also be called a ‘shock absorber’ for our body. The meniscus carries more than 50 % of the total load of the knee and is an important ‘bodyguard’ of the cartilage surfaces. Accelerated wear of the cartilage surfaces of the knee often occurs after meniscal injuries in combination with inadequate muscle statics or inadequately performed rehabilitation.
The medial and lateral meniscus provide greater compression resistance to the knee joint through the mechanism of distribution within the joint load to a ‘gross’ larger surface area. The meniscus straightens or aligns the end parts of the femur and tibia so that the force is transmitted through a larger surface are. It is important to understand that the meniscus is primarily an amplifier of vertical loads, while greater rotational, valgus and varus loads are the ‘Achilles heel’ of the menisci.
The meniscus is also an important ‘lubricant’ of the knee joint. Synovial fluid is the main lubricant of the joints, the menisci distribute the synovial fluid in the knee in proportion to the areas of stress.
Is the meniscus also a stabilizer of the knee?
The meniscus is indirectly an important stabilizer of the knee joint, as it achieves a more stable behavior of the knee joint during movement by distributing vertical loads over a larger gross surface. The meniscus also improves the stability of the knee joint with the specific structure of its growths, which are explained below.

Meniscus structure and terminology
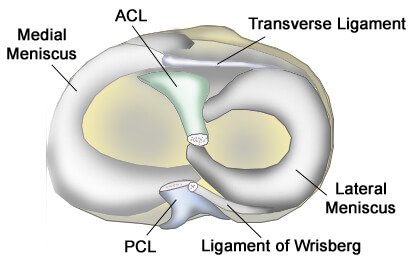
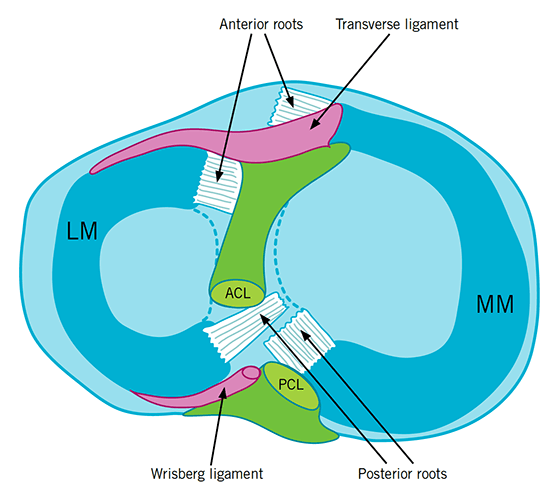
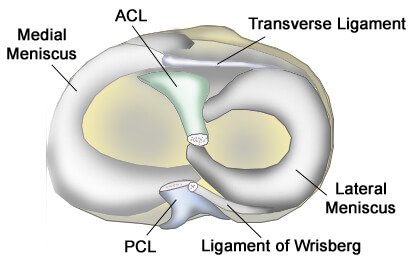
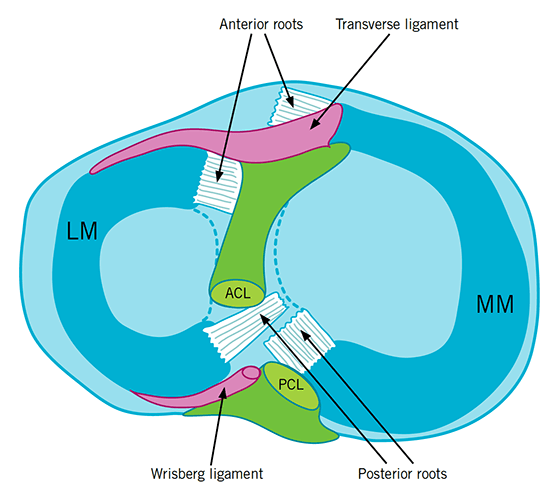
When reading magnetic resonance imaging (MRI) findings, we often encounter interesting terminology related to the menisci. We give you a real-time explanation of the anatomy of the meniscus. The meniscus has a complex anatomy of growths, which are often the cause of various types of meniscus damage. When reading the findings, you will often come across the term lesion – meaning injury and the term fissure – meaning a crack, and in relation to menisci also horn – meaning only part of the meniscus. Anterior horn means the front part of the meniscus. The posterior horn means the back part of the meniscus.
The medial and lateral menisci are connected inside the knee by the transverse ligament. The semimembranosus muscle (the hamstring muscle) and the quadriceps femoris muscle (the front thigh muscle) are both attached to the both menisci.
Medial meniscus
The medial meniscus is about 4.4 cm long, 3.5 cm wide and covers 50-60% of the surface of the medial plateau of the tibia, the anterior horn of the meniscus (anterior part) rises to the anterior part of the tibia.
The medial meniscus is the thickest at the posterior horn (back part) and becomes thinner toward the anterior horn. The posterior horn of the meniscus is most stressed during deep flexion (bending) of the knee. At maximum knee flexion, e.g. we notice that the posterior horn of the meniscus can slide over the edge of the tibial plateau, a large load occurs there, so e.g. in the acute postoperative phase of the meniscus, deep flexion of the knee is prohibited.
The medial meniscus has a total of three points of attachment, the lateral meniscus has only two points of attachment. The medial meniscus attaches to the front of the tibia, the joint capsule and the medial collateral ligament (MCL) and is generally less movable and more fixed than the later meniscus.
Did you know?
That the growth of the medial meniscus has at least 5 different anatomical variations of the anterior horn and at least 4 different anatomical variations of the posterior horn. This means that our menisci are genetically very different, which we are aware of at the Medicofit clinic. This is why we adjust the treatment of each meniscus individually.
Lateral meniscus
The lateral meniscus is long approximately 3.6 cm and 2.9 cm wide, but it covers a much larger area of the tibial plateau than the medial meniscus, up to 68%. The lateral meniscus is more mobile than the medial meniscus and is less often injured, it has only 2 attachment points, which allows it to move more.
The anterior (front) processes of the lateral meniscus are closer together than the medial meniscus, anteriorly the lateral meniscus grows onto the anterior cruciate ligament (ACL). The bony outgrowths of the anterior and posterior horns of the meniscus are connected via ligaments to the popliteus muscle, which enables the lateral stability of the lateral meniscus. In the posterior horn, the posterior part, the lateral meniscus ascends to the posterior cruciate ligament (PCL) via the ligament of Wrisberg.
The lateral meniscus is less firmly attached to the lateral part of the knee than the medial meniscus to the medial part of the knee, which is the reason for the greater number of medial meniscus injuries. The lateral meniscus can move up to 11 mm during movement.
Did you know?
That the lateral meniscus also has many anatomical variations of growths and that in some cases the bony growth of the posterior (back) horn of the meniscus is completely absent and all posterior stability is provided only by the Wrisberg ligament. At the Medicofit clinic, we put individual treatment first, we understand that the meniscus is a structure in which treatment methods must be strongly adapted to the type of meniscus injury.
How is the meniscus damaged?
The meniscus is most often injured in athletes, e.g. football, basketball, handball, also martial arts and skiing. It is often injured by falls on the knee or a blow to the knee. Meniscus injuries are characterized by two mechanisms of origin.
The meniscus can be damaged gradually due to long-term overloads, in which case it is a degenerative origin of meniscus damage. The meniscus can also be damaged traumatically, in which case it can be a contact or non-contact injury. The mechanism of meniscus injusty is usually strong rotation of the knee against a fixed foot.
A traumatic injury to the meniscus is characterized by severe pain, but it is not necessarily a rupture or tear. However, it is common for a traumatic injury to the meniscus to cause the inability to put weight on the leg and swelling of the knee. A bang is also often heard and the feeling that something has ‘broken off’, in this case it is probably a more extensive injury, e.g. rupture of the meniscus. Sport injuries to the meniscus are also characterized by the fact that athletes with a higher pain threshold can also continue their sports activities.
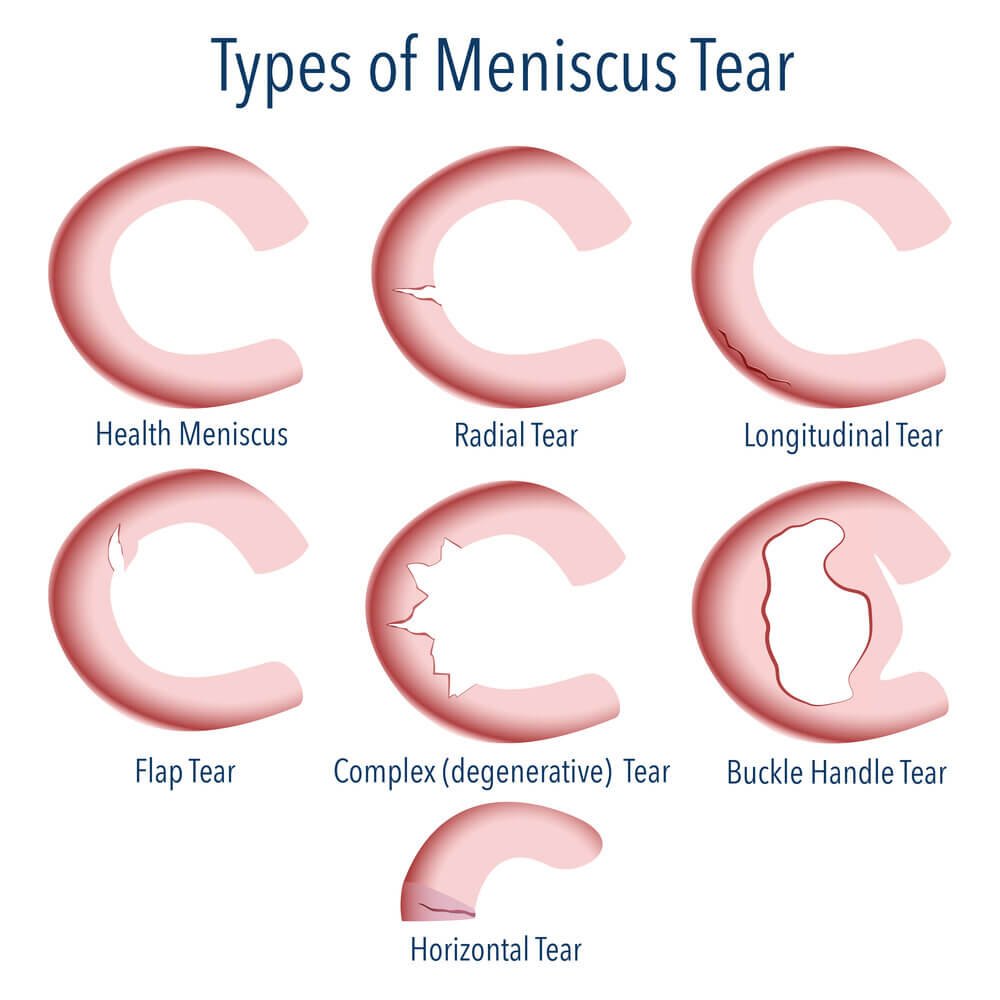
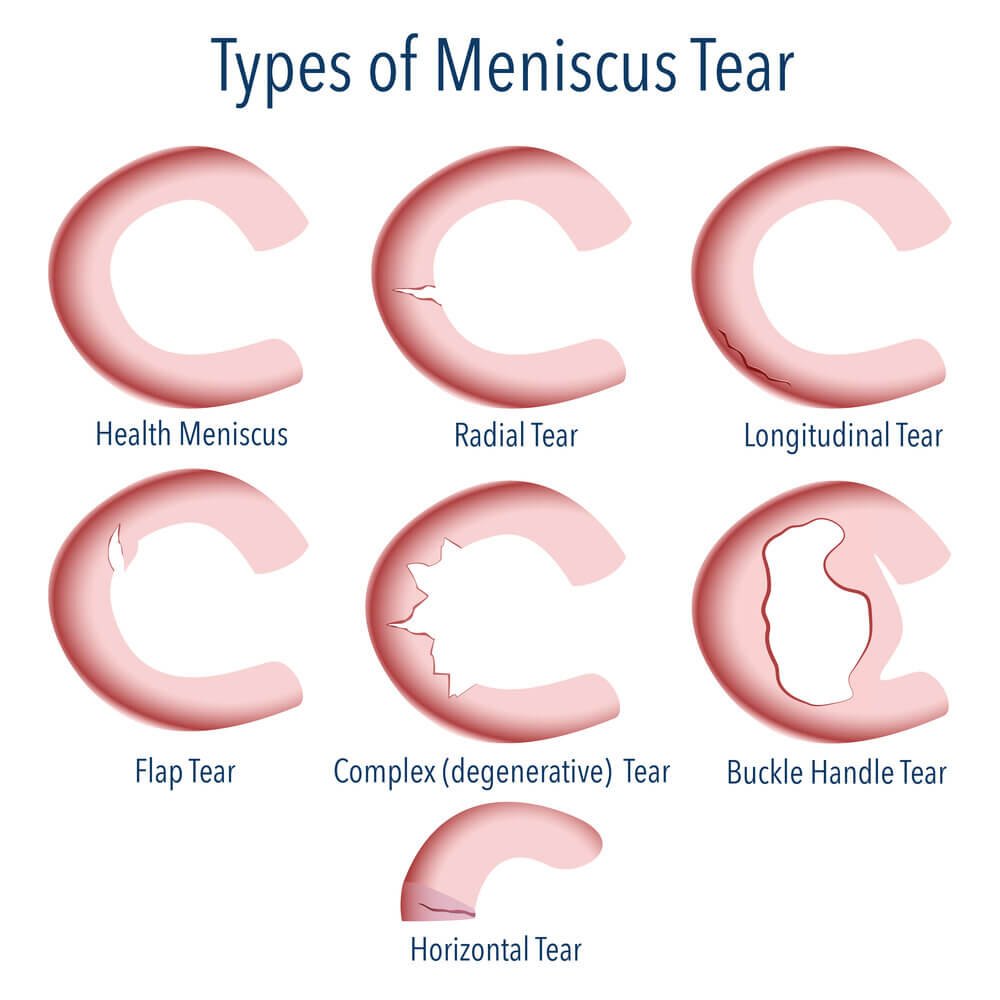
Degenerative damage to the meniscus occurs because the meniscus loses its resistance due to wear and tear and gradually becomes thinner, which then results in minor tears or cracks. In degenerative meniscus injuries, a free fragment of the meniscus (a free body) can often form, which breaks away from the main structure and ‘floats’ independently in the joint. In the following, we also explain meniscus impingement.
Due to its complex structure, the meniscus can be damaged in many different ways. It can be for e.g. squeezed, it can tear on the periphery in the red zone (the zone where it is blood-stained and heals), it can tear in half, there can be a loose body part of the meniscus, the edge of the meniscus can simply ‘roll’ over, the medial meniscus is characterized by ‘bucket handle tear’ rupture, when the meniscus is divided into two parts due to a longer longitudinal tear, and an empty space in the shape of the letter C is created in between. We know at least 6 different basic injuries of the meniscus and further on at least 12 well-known subvariations.
Is the medial meniscus or the lateral meniscus more often injured?
The medial meniscus is injured up to 6 times more often than the lateral meniscus. The difference is mainly due to the specific anatomical structure of growths, which is described at the beginning of the article. The medial meniscus is more strongly attached to the knee joint, has 3 attachment points and a lower degree of mobility than the lateral meniscus.
The medial meniscus grows on the MCL (medial collateral ligament), which is a commonly injured knee ligament in athletes. The lateral meniscus is more movable than the medial meniscus, so it is injured less often, but it is typical that injuries to the lateral meniscus are more complex and are more often treated surgically. The lateral meniscus is often injured when there is a stronger traumatic injury to the anterior cruciate ligament.
Does the damaged meniscus heal?
The blood supply to the menisci is poor, both menisci are well blooded at birth and later on, but only the outer edge of the meniscus, which is called the red zone, remains bloodied. If the meniscus is damaged in the red zone, there is potential for healing, but it depends on the physiotherapy and kinesiology.
Physiotherapy in the form of instrumental therapy to promote healing is essential for all patients who have an injury in the red zone of the meniscus. Instrumental therapy includes Laser, TECAR and magnetic therapy.
Book an appointment for meniscus rehabilitation
Is it absolutely necessary to operate on the meniscus?
Surgical treatment of the meniscus can be carried out in the form of partial meniscectomy – partial meniscectomy is the partial removal of the damaged part of the meniscus or in the form of suturing the meniscus, if it is a major injury or rupture, often with a ‘bucket handle tear’ type of meniscus injury. Rehabilitation after suturing the meniscus is more complex and has a longer acute phase with a longer phase of mandatory non-loading of the knee.
Urgent indications for meniscus surgery are rare, when it comes to mechanical symptoms in the form of knee sticking and painful knee skipping, surgical treatment is indicated. When it comes to a more extensive tear, surgical treatment in the form of suturing is indicated. Mere pain is not an indication for surgical treatment of the meniscus, just as minor damage or degenerative damage to the meniscus is not necessary indication for surgery.
Studies between 2012 and 2020 found that in meniscectomies (partial removal of the meniscus) compared to conservative treatment in the form of physiotherapy and kinesiology, there are no major differences in the function of the joint after 3 – 5 years from the onset of the injury or symptoms. Conservative treatment of the meniscus often has better effects for the patient in the long term as it improves its function and reduces the likelihood of progression of meniscus damage.
Removal of the meniscus means that there is a risk of knee arthrosis and accelerated cartilage wear at the site of removal. In any case, the first method of treatment for a minor meniscus injury is always physiotherapy and kinesiology.
Surgical treatment of minor lesions and injuries of the meniscus is advised only after at least 3 months of structured treatment in the form of physiotherapy and kinesiology has not significantly improved the pain symptoms or knee swelling.

How do we treat the meniscus at the Medicofit clinic?
At the Medicofit clinic, we carry out a complete clinical diagnosis of the damaged meniscus and first identify the symptoms and mechanical properties of your meniscus. Physiotherapy and kinesiology treatment methods are highly dependent on the type of injury you have.
In the case of most meniscus injuries, by improving muscle symmetries, we achieve greater stability of the damaged meniscus and more optimal kinematics of the knee joint. With instrumental physiotherapy, we act as an analgesic in case of pain. In case of degenerative damage to the meniscus in the red zone, we perform therapy that accelerates healing.
We put active physiotherapy first, so we direct the treatment towards obtaining the maximum function of your knee joint. It is important that the proprioception of the knee is good (position perception), and for all athletes, the ‘return to sport’ phase of rehabilitation is crucial, in which we perform specific testing for each sport and assess when the athlete is ready for full sports load after a meniscus injury.
When is it necessary to start physiotherapy?
In case of meniscus injury, we recommend acute physiotherapy, which should start no later than 7 days after the meniscus injury, ideally already 3 days after the injury. A common mistake patients make is to simply rest and avoid instrumental therapy to promote healing and therapy to maintain muscle activation.
In the case of meniscus surgery, we recommend pre-operative preparation in the form of targeted exercise to build muscle strength reserves, thereby preventing muscle atrophy after surgery, and in the form of neurostimulative exercise to maintain the maximum level of muscle activation.
At the Medicofit clinic, preoperative preparation for an injured meniscus is usually performed within a time window of 8-12 weeks.
Book an appointment for meniscus rehabilitation!
What do patients need to know about meniscus surgery?
The first treatment of the meniscus should always be conservative in the form of physiotherapy and kinesiology. At the Medicofit clinic, we are surprised that many patients seek surgical treatment before any conservative treatment. Such a procedure usually results in a rapid recurrence of the meniscus injury, as methodical physiotherapy is necessary to ensure optimal muscle function that stabilizes the knee joint.
Patients with meniscus damage must necessarily perform physiotherapy and kinesiology as the first choice of meniscus treatment, and in the case of indicated surgical treatment, physiotherapy and kinesiology in the form of preoperative preparation of the knee joint.
Patients should start physiotherapy early after the operation, if they have to wait for an appointment because of a work assignment, they should start physiotherapy already within the framework of a private clinic. The maximum regression or the setback of rehabilitation results in prolongation of the first acute phase of rehabilitation.
Rehabilitation of a meniscus injury takes 12-15 weeks and includes a progressive escalation of exercises until the patient is ready for full loads. Even in the case of not engaging in sports, the knee joint needs to be optimally strengthened.
It is necessary to preserve the meniscus for as long as possible at any cost, because at the place of removal, wear and tear of the knee and osteoarthritis develop rapidly. Studies clearly show a proportional correlation between the amount of meniscus removed by meniscectomy and the likelihood of developing knee osteoarthritis.