For all athletes and those who live an active lifestyle, it is important to be aware of the various symptoms that signal a knee injury. It is even more important that you know what to do according to the onset of symptoms and what treatment is optimal for you. Remember that minor pain that appears for the first time can be a sign of the beginning of a major injury.
Here is a brief overview of 7 knee injuries that are common athletes:
- Patellar Fracture
- Knee Dislocation
- Jumper’s knee
- Knee ligament injuries
- Meniscal Injury
- Iliotibial Band Syndrome
- Bursitis
In the following, we will take a closer look at each of the injuries listed above.

Patellar fractures are more serious injuries to the knee, which can cause profound damage to the mechanics of the joint. This happens when you fall directly on the knee (direct trauma e.g. hit with a hockey stick) or due to sudden overuse. If the amount of stress is greater than what the patella can withstand, the force causes a fracture.
Symptoms of a patellar fracture
Symptoms include:
- Sudden onset of sharp, intense pain in the front of the knee
- Swelling
- Palpable deformity on the knee cap
- Inability to lift the foot
- Obvious deformity (in severe cases)
Diagnosis and treatment of patellar fracture
The diagnosis is established by finding out how the injury occurred, through a clinical examination and radiological examinations. Treatment may include realignment of the patella, surgical reconstruction, and the use of protective assistive devices (knee braces, casts, or crutches). Athletes are rehabilitated by gradual conditioning of the knee joint with safe and properly progressed exercises.
Athletes with a fractured patella usually make a full recovery with proper treatment. They can resume sports within a few months under the precise guidance of a specialist physiotherapist and kinesiologist. If a patellar fracture is poorly rehabilitated, it often develops into other secondary pathological conditions such as post-traumatic arthritis, chondromalacia or patellofemoral pain syndrome (PFBS) and jumping knee.
Knee dislocations can be divided into high-velocity and low-velocity causes. High-speed knee dislocations are usually the result of an aggressive force, such as e.g. traffic accidents and running into the knee while sprinting. Low-velocity knee dislocations are common in sporting situations.
In athletes, knee dislocation occurs when the foot is placed on the ground during a quick change of direction or twisting of the knee, or during falls. This is common in sports such as football, cycling, skiing, gymnastics and long jump.
Symptoms of a sprained knee
Symptoms include:
- Rapid, acute swelling
- Severe pain and tenderness
- Hypermobile patella
- Obvious knee deformity
- Loss of feeling or pulse below the knee
Diagnosis and treatment of knee dislocation
After suspecting a knee dislocation, the doctor first checks the distal heart rate, especially in the foot, as vascular damage is a common associated trauma in knee dislocation. An X-ray is taken to assess the extent of bone damage.
Treatment usually involves repositioning the patella (moving the patella back into the groove), surgery (reconstructing the joint capsule), and immobilizing the joint. A sprained knee is categorized as a more serious injury.
Professionally managed rehabilitation is the key to complete rehabilitation of a dislocated knee. A dislocated knee rarely regains the same load-bearing capacity as before the injury, but this is possible with well-progressed specialized exercise in the second phase of rehabilitation.
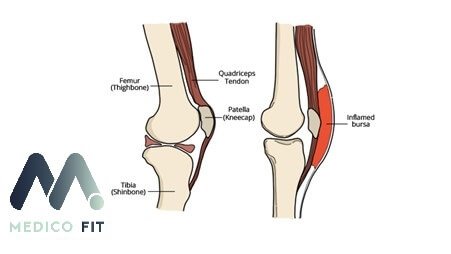
Knee bursae are fluid-filled sacs located near the knee joint. When functioning correctly, they help the articular surfaces slide smoothly and prevent bone structures from damaging muscles and ligaments.
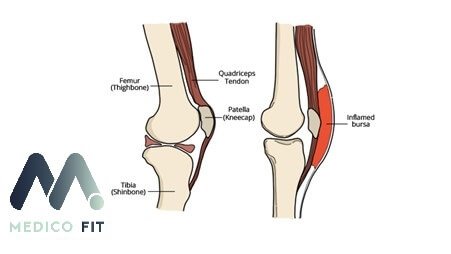
Knee bursting occurs when one or more bursae become irritated, inflamed, or damaged. Prolonged pressure, traumatic impacts, and repetitive motive (e.g. running) can cause irritating friction that causes bursitis. It is characteristic of bursitis that it worsens if the joint has been held in one position for too long.
Symptoms of bursitis
The main symptoms include:
- An initial sharp or stabbing pain followed by a dull ache
- Swelling and redness on the front of the knee
- Heat around the joint
- Pain when kneeling
- Increased discomfort after prolonged rest of the joint
- Difficulty extending or bending the knee
Diagnosis and treatment of bursitis
Bursitis can sometimes be confused with some other knee problems, such as arthritis, stress fractures, and tendonitis.
In order to properly diagnose the condition, a physical therapist or orthopaedic doctor will perform a thorough evaluation with clinical tests and differential diagnosis,which includes MRI, X-ray and ultrasound.
In most cases, knee bursitis disappears with properly performed conservative rehabilitation with physiotherapy. In some cases, it can be more severe and require medical attention, and the intervention is mainly aimed at alleviating the symptoms.
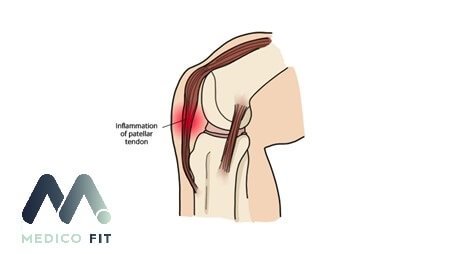
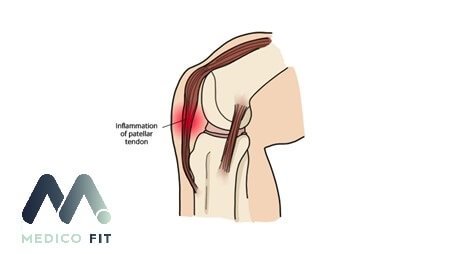
Patellar tendinopathy, also called jumper’s knee or ‘jumper’s knee’, is a degenerative overuse injury characterized by pain in the front of the knee.
Athletes get this type of injury in sports where there are frequent jumps or landings (e.g. volleyball, basketball, long jump, also football, ski jumping and martial arts). It mainly occurs when you suddenly expose your body to a rapid increase in training load or when you train on hard surfaces such as concrete or, in football, artificial grass.
Excessive mechanical stress on the patellar ligament causes tiny tears in the collagen fibers and, as a result, an inflammatory and painful reaction to additional loading.
Jumper’s knee usually occurs gradually.
Athletes with mild to moderate symptoms of jumper’s knee often continue to train and compete, which is often a fatal mistake in terms of successful treatment. At the first appearance of the signs of jumping knee, it is important that the degenerated fibers heal well, as this prevents further problems. When training continues, the fibers are often damaged to the point where complete healing is severely limited and can take from several months to several years.
It is characteristic of jumper’s knee that the longer the condition is present, the more quickly the symptoms appear, and the longer the healing time.
Often for the jumper’s knee, it is not a responsible approach in early rehabilitation and at the first appearance of symptoms it leads to permanent deterioration and dysfunction.
Symptoms of Jumper’s Knee
These include:
- Pain and tenderness below the knee
- Pain that gets worse when jumping, landing, running, or sitting for long periods of time, even when walking down the stairs
- Weakness, stiffness and weakness in the knee
Diagnosis and treatment of jumper’s knee
For diagnosis, a visit to a physiotherapy specialist is required, when he will assess or refute the presence of tendinopathy with clinical and motor tests. Visiting standard diagnosis in this case in this case is not always a reliable method and often greatly increases the time until the correct diagnosis is confirmed.
Patellar tendinopathy is characterized by pain symptoms on the front of the knee, just below the kneecap – the patella. The rapid onset of symptoms after motor tests performed to provoke patellar pain is very characteristic.
Jumper’s knee is perhaps the condition that is most frequently misdiagnosed, incorrectly treated, or has too long a waiting window for the right diagnosis, out of all the conditions considered in the modern medical profession. Jumper’s knee is a condition where acute treatment has the least effect on long-term performance, the application of exercises to eliminate the risk factors that cause the trigger of jumper’s knee is key.

Ligaments are tough connective structures that surround the joints, provide them with support and structure, and control the movement itself. Ligament injuries often occur as a result of traumatic sports injury, causing the knee joint to become severely weakened and unstable. Ligament injuries also severely limit knee movement.
The knee is stabilized by 4 main ligaments that connect the femur and tibia:
- Anterior Cruciate Ligament (ACL) – A ligament in the center of the knee that controls rotation and forward movement of the tibia.
- Posterior Cruciate Ligament (PCL) – A ligament in the center of the knee that controls the backward movement of the tibia
- Lateral Collateral Ligament (LCL) – the ligament responsible for external stability of the knee.
- Medial Collateral Ligament (MCL) – the ligament responsible for the internal stability of the knee.
When any of the four ligaments is damaged, the knee is typically unstable in the direction in which the damaged ligament stabilizes it.
There are four clinical tests for assessing knee ligament injuries: Anterior Dawer Test (for ACL), Posterior Dawer Test (for PCL), Valgus Stress Test (for MCL) and Varus Stress Test (for LCL).
Types of knee ligament injuries
- ACL Injury – Rupture, partial rupture or strain of the ligament due to a sprained knee, a strong forward movement of the joint, due to a sudden stop or change of direction, due to improper jump and landing mechanics. ACL injury is common in sports such as skiing, basketball, soccer, volleyball, handball and combat sports.
- PCL Injury – the strongest ligament in the knee can be stretched or torn by a sharp, forceful blow to the front of the shin, often during a forward tackle in football.
- LCL Injury – the LCL can be injured during activities that involve twisting, bending, or rapid change of direction. This injury is common in sports where there are strong varus loads on the knee or bumps into the inside of the knee, e.e. in football.
- An MCL injury – often called an MCL sprain, is the result of a direct blow to the outside of the knee, such as when playing football or hockey.
Knee ligament injuries have the following typical symptoms:
- A loud pop or snap at the time of injury
- Sudden and severe pain that prevents you from continuing your activity after the injury
- Black-blue colouration around the knee
- Knee instability
- Swelling in the first 24 hours after the injury
- A feeling of looseness in the joint
- Inability to put weight on the affected joint due to pain
Diagnosis and treatment of knee ligaments
To diagnose ligament damage, the doctor begins with a physical examination and application of clinical tests. They will examine the knee for swelling and tenderness. The procedure can be uncomfortable because it involves various knee movements to assess the range of motion and external pressure on the knee, imaging and X-ray diagnostics are also performed.
The extent of ligament damage is classified according to the grading system, grade I (mild), grade II (moderate) and grade III (severe).
The duration of the treatment depends on the type and severity of the injury, especially on the extent of the damage to the ligamentous apparatus.
Most collateral ligament tears (LCL and MCL) usually do not require surgery, well-executed rehabilitation with physiotherapy and kinesiology is sufficient. In cases where the cruciate ligament (ACL or PCL) is torn and stretched beyond capacity, ligament reconstruction is often the recommended form of treatment.
After reconstruction of the knee ligaments, rehabilitation with physiotherapy and kinesiology usually takes 6-9 months until full recovery.
Illiotibial tract syndrome
Iliotibial tract syndrome outline medicofit
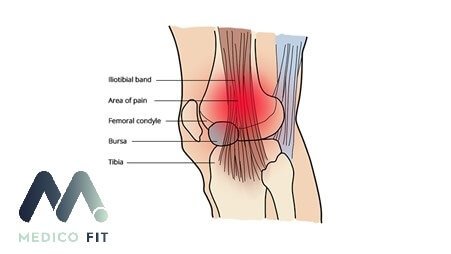
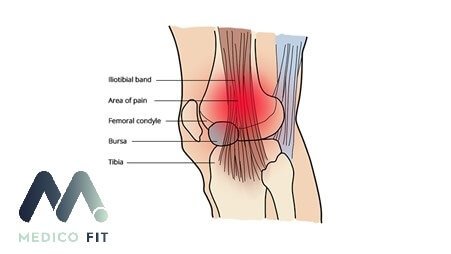
The iliotibical tract, or iliotibial band (ITB), is a thick band of fascia that runs along the outer length of your thigh to the top of your shin. It is made up of dense fibrous connective tissue that extends from the hip joint and rises on the lateral side of your knee.
The ITB and its associated muscles work to extend, abduct, and laterally rotate your hip.
Iliotibial band syndrome is considered a nontraumatic overuse injury associated with underlying hip abductor muscle weakness. Overuse is the result of repetitive bending and extension of the knee, causing pain on the outside of the knee, usually in cyclists and runners. It is also associated with other activities such as hockey, swimming, hiking, basketball and soccer.
Symptoms of iliotibial tract syndrome include:
- Pain and/or tenderness on palpation
- Prolonged pain after exercise
- A clicking sensation on the outside of the knee
- Warmth and redness around the outside of the knee
Diagnosis and treatment of the iliotibial tract
A diagnosis is made based on a medical history that details your health problems and current symptoms. This will also include a physical examination and a thorough assessment of the range of motion and strenghth of your knees by a physiotherapist.
Using certain clinical tests, a physical therapist can differentiate between iliotibial tract syndrome and other possible causes of knee pain (e.g. osteoarthritis, meniscal tear).
For successful treatment, it is necessary to limit provocative activity for a while, e.g. running to reduce pain irritation, prevent further injury and allow the knee to heal completely. In the acute phase, instrumental physiotherapy is performed, and in the following, kinesiology exercises are used to eliminate the risk factors that caused the injury to the iliotibial tract or ITB syndrome.
Most patients recover from iliotibial band syndrome within 12 weeks, but it usually takes several months to return to full competitive activity without pain.

The meniscus is a crescent-shaped cartilage pad in the knee that acts as a shock absorber for vertical forces. Meniscus tears are considered a very common knee injury and are the result of a sudden twist or significant trauma, especially in sporting circumstances.
A meniscus injury can occur alone or in combination with associated ligament injuries. Meniscal injuries can range from minor to extensive, depending on the extent of tissue damage.
Symptoms of a damaged meniscus include:
- Localized pain on the medial or lateral side of the knee
- Locking and clicking sensations in the knee
- Delayed intermittent knee swelling
Diagnosis and treatment of meniscus
A torn meniscus is diagnosed based on a thorough history and clinical examination. To confirm the diagnosis, it is necessary to undergo imaging tests such as MRI, X-ray or arthroscopic examination.
Immediate treatment for meniscus injuries includes the RICER method (rest, ice, compression, elevation, and referral to a rehabilitation specialist).
It is important that this protocol is followed only within 48-72 hours, primarily to reduce pain and as a management of the acute post-traumatic condition until a visit to medical care.
We also use the NO HARM protocol – no heating, no alcohol, no running or activity, and no massage – until the visit to medical care. This helps to reduce the swelling and bleeding of the injured knee.
With physical therapy or physiotherapy can be used to strengthen the muscles around the knees and legs to build stability and support for the knee joints. The patient may need to wear a knee brace that is specially designed to support the meniscus injury. The indication for surgery is a mechanical symptom in the form of knee stiffness, which does not disappear during rehabilitation and limits the normal function of the knee.
Rehabilitation of the meniscus is possible with an operative or conservative physiotherapy approach. It depends on the extent of the meniscus damage. Athletes can return and compete in their sports after a meniscus injury and successful rehabilitation. A key part of the rehabilitation of meniscus injuries in athletes is building a strong preventive base to prevent repeated meniscus injuries that can result in degeneration of cartilage surfaces.
Knee injuries – conclusion
With this knowledge, we hope that you will become successful in preventing and eliminating the symptoms of knee joint injuries. Especially in the event of an injury, do not wait and visit a specialist who will provide a correct diagnosis. Don’t wait for your knee injury to get worse and don’t let the pain limit your athletic performance.