The complexity and diversity of the hip joint is reflected not only in the tasks it performs, but also in the pathological changes that can affect it. (13).
These changes are often accompanied by hip pain, affecting both the general population and athletes. Age, gender, genetics, lifestyle, work stress and sport contribute to the development of certain pathologies (9).
Functions of the hip joint
The hip joint is designed to carry loads and ensure mobility of the lower extremities. It has three fuctions:
- Allows lower limb mobility,
- Transfers loads between the upper body, trunk and lower limbs, and
- Provides stable support for activities involving self weight bearing (2).
The hip is designed to ensure the smooth performance of the tasks described above. The pelvis is made up of three bones, which meet at a hollow on the outer part of the pelvis. This is the socket where the femoral head joins the femur and together they form the hip joint (6). The hip joint is a ball and so has a fairly large range of movement in all planes.

The movement requires a complex system of passive and dynamic stabilisers. Due to the large range of motion of the hip joint, a large number of muscles pass through the hip joint to provide movement and stability. The hip muscles grow from the pelvis and lumbar spine and attach to the femur and also to the calf bones (13).
The hip joint is never fully unloaded during daily activities (9). To limit pain or possible joint wear, the impact of the reaction force on the joint should be reduced, which means, among other things, reducing body weight (if necessary) and developing inter-muscular coordination to achieve a coordinated neuromuscular system, thus placing a more even load on the joint (9). This can be achieved through physiotherapy and kinesiology.
Sometimes hip pain is caused by malformed bones, or the bones wear down so much over time that surgery is unavoidable. In these cases, physiotherapy and kinesiotherapy in rehabilitation will also successfully help to regain function and live a life with less pain.
Making the right diagnosis
When hip pain is present, you need to analyse your whole body well – both in static posture and during movement. There can be many different causes of hip pain, just as there are many different anatomical structures in the hip area.
The impact of adjacent decisions should not be overlooked in the review. Hip pain may be secondary to the knee joint, ankles or feet. It is also important what happens higher up the hip joint – in the trunk.

The description of the pain also helps physiotherapists to make a diagnosis. At the examination, try to describe to the physiotherapist what the hip pain is like in terms of intensity, duration, location and quality.
Pain intensity
The physiotherapist will be interested in how severe the pain is and when it occurs. Pain is usually rated from 0 – 10, with 0 being no pain and 10 being the worst pain imaginable.. Another important piece of information is what makes the pain worse and what relieves it. When aggravated during movement, it causes muscle tension, which can lead to soft tissue damage. During movement, we also exert a compressive force on the joint, which can be painful if the articular surfaces (bone, cartilage) are damaged.
If you experience hip pain at night, the trigger may be the position of your body during sleep. If bursitis is present, sleeping on the affected hip may provoke irritation and consequent night pain. Similarly, in osteoarthritis or piriformis syndrome, prolonged positioning alone can provoke hip pain at night. Tendinopathies can also be a cause of hip pain at night. Tendons are known to heat up during activity and the pain subsides. The pain appears after 24 hours after the activity.
Duration of pain
Depending on the duration, a clinical distinction can be made between acute pain, which is present for less than 3 months, and chronic pain, which is present for more than 3 months.
From the information on how long the pain in the hip has been present, we can understand whether it is an injury that happened at a specific moment, e.g. fractures, muscle or tendon tears, or a degenerative condition that gradually worsens, such as osteoarthritis.
Location of pain
The cause of hip pain can be from various structures. It is also important to know whether the pain is present only locally/pointwise or if it may spread to neighbouring areas. If there is a nerve damage, it is characteristic that it is felt along the entire course of the nerve. If, for example, pinched sciatic nerve, we will feel the pain right down to the big toe. For additional confirmation of the diagnosis, after consultation with a specialist, it is recommended to undergo diagnostic imaging according to the pathology.
Pain quality
The quality of the pain is also very important, meaning how the pain is felt: is it sharp, dull, deep, superficial, burning, etc. This information will better guide the physiotherapist as to which hip structure is damaged.
Burning pain in the hip may be present for a number of different reasons. It could be bursitis, tendinitis, muscle or nerve damage. Burning pain in the hip is felt as a strong, sharp, cutting pain and is often accompanied by inflammation. Burning pain in the hip is common in the diagnosis of bursitis, compression syndrome and osteoarthritis, where damage to the articular surfaces occurs due to increased friction.
Changes in joint surfaces can also lead to changes and inflammation in tendons or muscles. Burning pain in the hip also accompanies conditions where there is nerve compression. Often, we also feel a tingling sensation, an altered sensation or numbness.
Possible diagnoses
Let’s take a look at some of the diagnoses in which hip pain is a constant companion as a consequence.
Arthritis
Arthritis is a term for inflammation of the joints and surrounding structures. There are many different types, the most common being osteoarthritis and rheumatoid arthritis, but arthritis also includes puerperosis and fibromyalgia (1). Osteoarthritis (OA) of the hip is a very common problem in Western society. It affects up to 25% of the population over 55 years of age, is more common in women, and genetic and lifestyle factors contribute to its onset, in addition to ageing. (10).
OA is a progressive wear and tear of the cartilage, resulting in bone-on-bone contact, which causes changes in the bone system. Of course, changes in the bone system. Of course, one change affects the other, and the soft-tendinous structures of the hip joint are also affected.
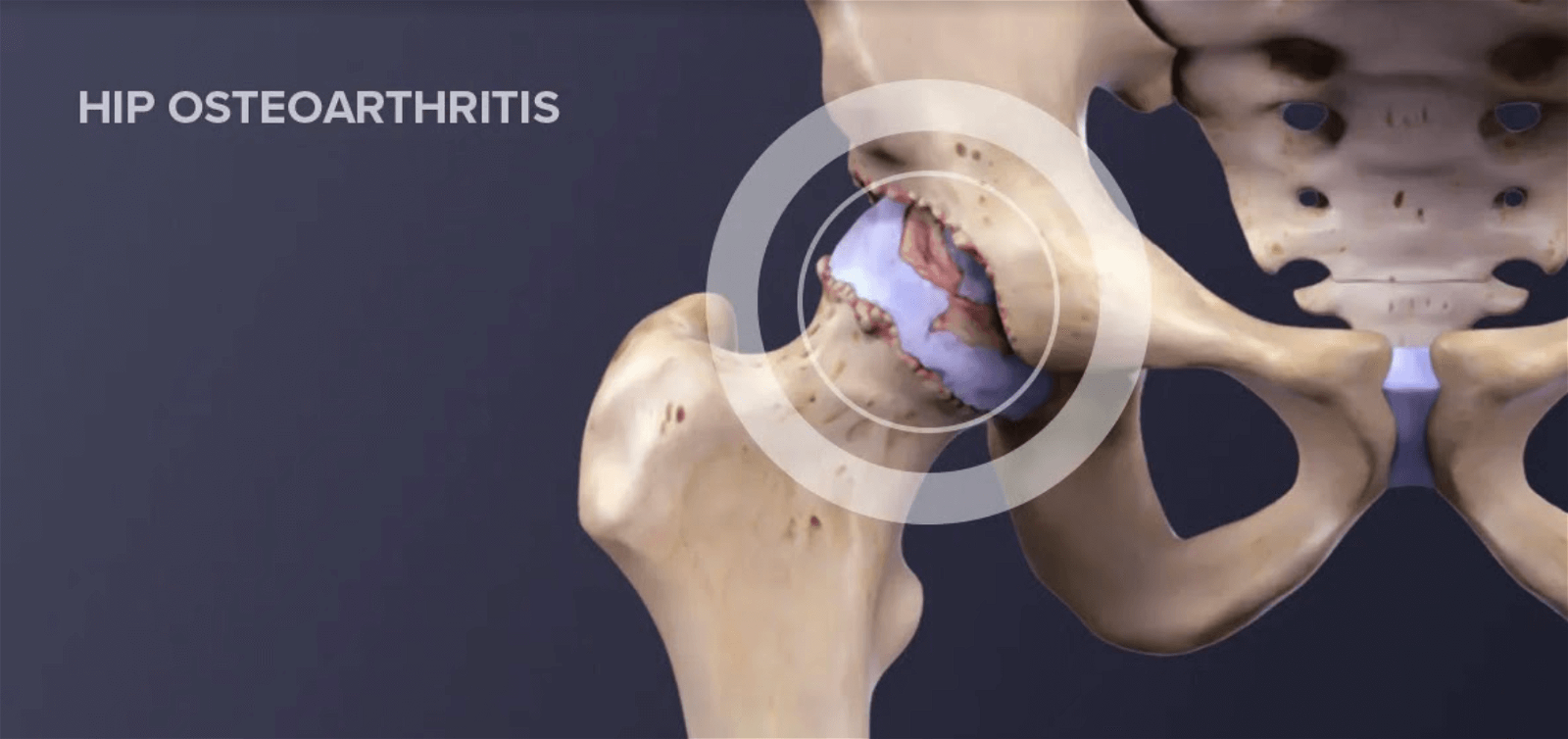
Hip pain that occurs in OA occurs gradually. May radiate forward into the groin or back towards the buttock, thigh or knee. Hip pain at night or at rest after activity is particularly common. It is also characterised by stiffness of the joint in the morning or after prolonged rest.
When patients perform active hip flexion, they feel pain on the outside of the hip. Symptomatology associated with hip pain includes the presence of popping, grinding, bouncing in the hip joint, limping, decreased joint mobility and increased tenderness. In the early stages of the disease, the greatest limitation occurs in abduction and rotation movements, but as the disease progresses, movements in other directions also become limited (1).
Hip dysplasia
Hip dysplasia is a condition comprising various abnormalities in the anatomical shape of the femoral head and the acetabulum, the joint cap with which the femur is in contact. Suboptimal bone formation eventually leads to chronic changes, manifested by changes in the bone system as well as in the joint capsule, ligaments and muscles of the hip.
Hip dysplasia is a common developmental abnormality and the most common musculoskeletal abnormality. Most (60-80%) abnormalities resolve spontaneously within 8 weeks after birth (14). Hip dysplasia is also seen during adult post-pupation. A few of them report problems from childhood, but most adults are unaware of a problem until they have hip pain.
Pain usually occurs on the lateral side of the hip or anteriorly in the groin. Pain is felt as deep, resulting from chronic damage to the cartilage, labrum or soft tissues on the lateral or anterior aspect of the hip. It usually increases during activity and decreases with rest.

Hip pain can also occur due to muscle overstrain. This is because the muscles that move the hip away (abductors) have to work harder because the acetabulum is more shallow in hip dysplasia and does not provide sufficient support for the femoral head. The hip flexors also need to be more active and sometimes hip pain is accompanied by a tightening, popping and bouncing sensation during activity. (8). Hip pain at night occurs in about half of cases of hip dysplasia. If you are experiencing it, see a specialist (7).
On average, it takes about 5 years for an adult with hip dysplasia to get the right diagnosis, during which time they see at least 3 different health specialists. So if your problems persist, if your hip pain is recurring and not getting better, get a second opinion as soon as possible (8).
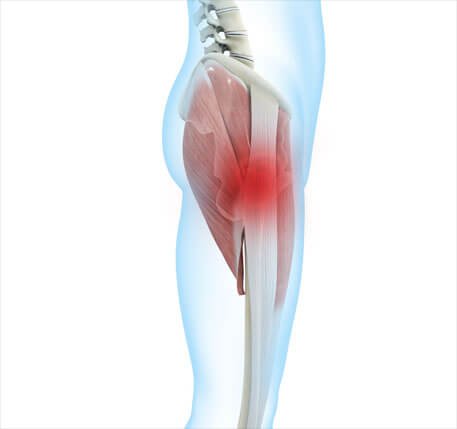
Piriformis syndrome
Piriformis syndrome is a neuromuscular disorder that occurs when the piriformis muscle compresses the sciatic nerve. The piriformis muscle is important in lower body movement as it stabilises the hip joint and helps to lift and rotate the thigh. The sciatic nerve runs along or through the piriformis muscle, down the back of the leg and ends in the feet. A spasm of the piriformis muscle can cause compression of the nerve and piriformis syndrome occurs (11).
Hip pain in piriformis syndrome occurs in the buttock and lateral aspect of the hip, but can occasionally be felt along the front of the thigh. Pain increases during activity, when getting out of bed or when sitting for long periods of time. It can be triggered by a specific movement that causes the pain to spread along the course of the sciatic nerve down the leg.
Individuals report tingling, sharp pain spreading up the leg and numbness in the buttocks. The pain can be very severe (11). It is often the case that piriformis syndrome is mistaken for sciatica, where there is pathology of the discs of the lumbar spine and, as a result, the nerve is compressed in the area of the spinal canal exit. They are distinguished by a good clinical examination and diagnostic imaging.
Oppression syndrome
Femoroacetabular impingement syndrome is also known as FAI. Similar to hip dysplasia, compression syndrome is caused by non-optimally shaped articular surfaces of the acetabulum or femoral head. FAI syndrome morphologically involves three variations in the shape of the articular surfaces.
The first form is that the femoral head is not perfectly round at the femoral neck and therefore smooth movement is not possible. When moving, it “hits” the cartilage inside the acetabulum and damages it, causing hip pain. The second form of FAI is that the acetabulum bone is shaped so that it extends beyond the edges of the normal shape – it encircles the femoral head too much, leading to increased friction and intra-skeletal injuries. The third form is a combination of the first two (5).

Hip pain associated with compression syndrome, either on the lateral side of the hip, in the groin or radiating to the buttocks, lower back and thigh. Pain usually occurs during movement and is usually accompanied by limitation of mobility, clicking, popping and bouncing in the joint, stiffness of the joint and reduced functionality.
Pain in the hip may be caused by too much friction between the bones (5). In FAI, hip flexion with internal rotation is often the most limited. This can cause problems when, for example, climbing or descending stairs, where more hip flexibility is needed than when walking on level ground. (15).
Greater trochanteric pain syndrome – GTPS
Greater trochanteric pain syndrome (GTPS) is an umbrella term that covers a variety of pathologies from bursitis to tendinopathies. It can result from tendon overload, incomplete and insufficient tendon healing, tendon compression due to asymmetrical action of the soft structures in the hip, prolonged static hip flexion (e.g. during sitting), muscle imbalance and thus overloading of certain structures, popping hip syndrome or as a consequence of hip osteoarthritis or iliotibial band syndrome (4).
Hip pain in GTPS is typically lateral. The area is extremely sensitive to touch, and the pain can spread down the lateral thigh towards the knee or back towards the buttocks.
The pain is described as stabbing and intense, and there may also be burning pain in the hip, which increases with the simultaneous movement of hip adduction and external rotation – i.e. the movement of trying to place the ankle of the leg on the opposite knee (4).
Hip pain is also aggravated when lying on the affected side, and sometimes lying on the unaffected side, where the painful leg falls slightly downwards, causing compression, is also problematic. Hip pain at night can therefore also be caused by compression syndrome. The pain is also expressed during activity, when the leg is put under strain – walking on flat ground or stairs, jogging, sometimes just standing is enough. Pain is also aggravated by prolonged sitting or sitting cross-legged (12).
Because of the complexity of the rehabilitation process, it is important who you trust with your body
Hip pain is a common accompanying symptom of various pathologies. As the body is a complex and coordinated system, it often happens that one pathology leads to another and we have a problem in several systems at the same time.
Hip dysplasia, for example, can lead to osteoarthritis accompanied by tendinopathy. At the same time, the altered dynamics of the hip affect the knee and the spine, and suddenly it is difficult to know how and where to tackle the problems that have arisen over the years. So don’t do rehabilitation on your own.
Book your physiotherapy appointment for hip pain now!
It is extremely important who you trust with your body in the rehabilitation process or in preventive exercise programs. Proper progression can only be carried out by a team of multidisciplinary specialists who work together, complement each other, understand the mechanism of injury and the specific sport or recreation to which the injured person is returning. The Medicofit private clinic has all of the above qualities.

References
1.American Academy of Orthopaedic Surgeons. Diseases and conditions: Osteoarthritis of the hip.Available at: https://orthoinfo.aaos.org/en/diseases–conditions/osteoarthritis-of-the-hip [20.9.2022]
- Brunker & Khan’s. Clinical sports medicine. Hip related pain. pp: 510-545.
- CDC, Arthritis types. Available at: https://www.cdc.gov/arthritis/basics/types.html [20.9.2022]
- Ganderton, C., Semciw, A., Cook, J., Moreira, E. & Pizzari, T.. 2018. Gluteal loading versus sham exercises to improve pain and dysfunction in postmenopausal women with greater trochanteric pain syndrome: a randomized controlled trial. Journal of Women’s Health. 1;27(6), 815-29.
- Griffin DR, Dickenson EJ, O’Donnell J, Agricola R, Awan T, Beck M et al.(2016).The Warwick Agreement on femoroacetabular impingement syndrome (FAI syndrome): an international consensus statement. Br J Sports Med. 50(19):1169-76.
- Hlebš, S., Slakan Jakovljević, B. & Klauser, M., 2014. Manualna terapija – sklepna mobilizacija udov testiranje in terapija. Univerza v Ljubljani, Zdravsvtena fakulteta, pp 86-87.
- International hip dyspalsia institute. Adult Diagnosis. Available at: https://hipdysplasia.org/adults/diagnosis/ [20.9.2022].
- International hip dyspalsia institute. If you have hip dysplasia, you are not alone. Avaliable at: https://hipdysplasia.org/adults/ [20.9.2022].
- Kodarin, Jan. 2017. Najpogostejše poškodbe kolčnega sklepa in gibalnoterapevtski pristopi k zdravljenju. Diplomsko delo. Koper: Univerza na Primorskem.
- Lespasio MJ, Sultan AA, Piuzzi NS, Khlopas A, Husni ME, Muschler GF, Mont MA. Hip osteoarthritis: a primer. The Permanente Journal. 2018;22. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5760056/ (last accessed 19.11.2019)
- Lightsey, R. (2021). Piriformis syndrome. WebMD. Available at: https://www.webmd.com/pain-management/guide/piriformis-syndrome-causes-symptoms-treatments [24.9.2022]
- Lin, C.Y. & Fredericson, M., 2015. Greater Trochanteric Pain Syndrome: An Update on Diagnosis and Management. Curr Phys Med Rehabil Rep, 3(1). 60-66.
- Moore, K.L., Dalley, A.F. in Agur, A.M.R. (2014). Clinically Oriented Anatomy. (7th ed.) Baltimore: Lippincott Williams & Wilkins, a Wolters Kluwer business.
- Radiopedia Developmental dysplasia of the hip Available: https://radiopaedia.org/articles/developmental-dysplasia-of-the-hip [20.9.2022].
- Wahoff, M., 2014. Rehabilitation after labral repair and femoroacetabilar decompression: Criteria-based progression through the return to sport phase. The International Journal of Sports Physical Therapy, 9(6), pp 813









