A herniated disc, or technically known as a “disc herniation”, is one of the most common specific low back pain, as it is accompanied by pathological conditions that can be detected with appropriate diagnostics. The main symptoms of a herniated disc include low back pain, pain radiating down the leg, and decreased muscle strength – symptoms collectively known as “sciatica”.
A herniated disc often occurs in adult population between the ages of 30 and 50, and it occurs even more frequently in top athletes, as they are constantly exposed to stresses on the spine.
It is a common pathological condition that occurs mostly in people with an inappropriate and sedentary lifestyle. A herniated disc occurs due to long-term stress on the spine (constant trunk flexion), and can also cause narrowing of the spinal canal (spinal stenosis) and nerve compression. The main symptom of a herniated disc is back pain, which can be severe and limiting.
Modern rehabilitation tends to treat the pathological condition of a herniated disc with specialised training, because in this case you can expect fewer complications and better long-term health of the spine – with appropriate rehabilitation, spinal surgery is required in less than 5% of cases.
A comprehensive approach to the rehabilitation of a herniated intervertebral disc eliminates the underlying causes of the herniated disc (sedentary lifestyle, muscle weakness, etc.), in addition to pain symptoms.
A herniated disc is a condition that occurs due to years of cumulative stress on the spine and requires a comprehensive approach to treatment. It is important who we entrust with our body during the rehabilitation process, as only trained experts can provide appropriate care and effective treatment.
Book an appointment for herniated disc rehabilitation
Basic anatomy of the spine
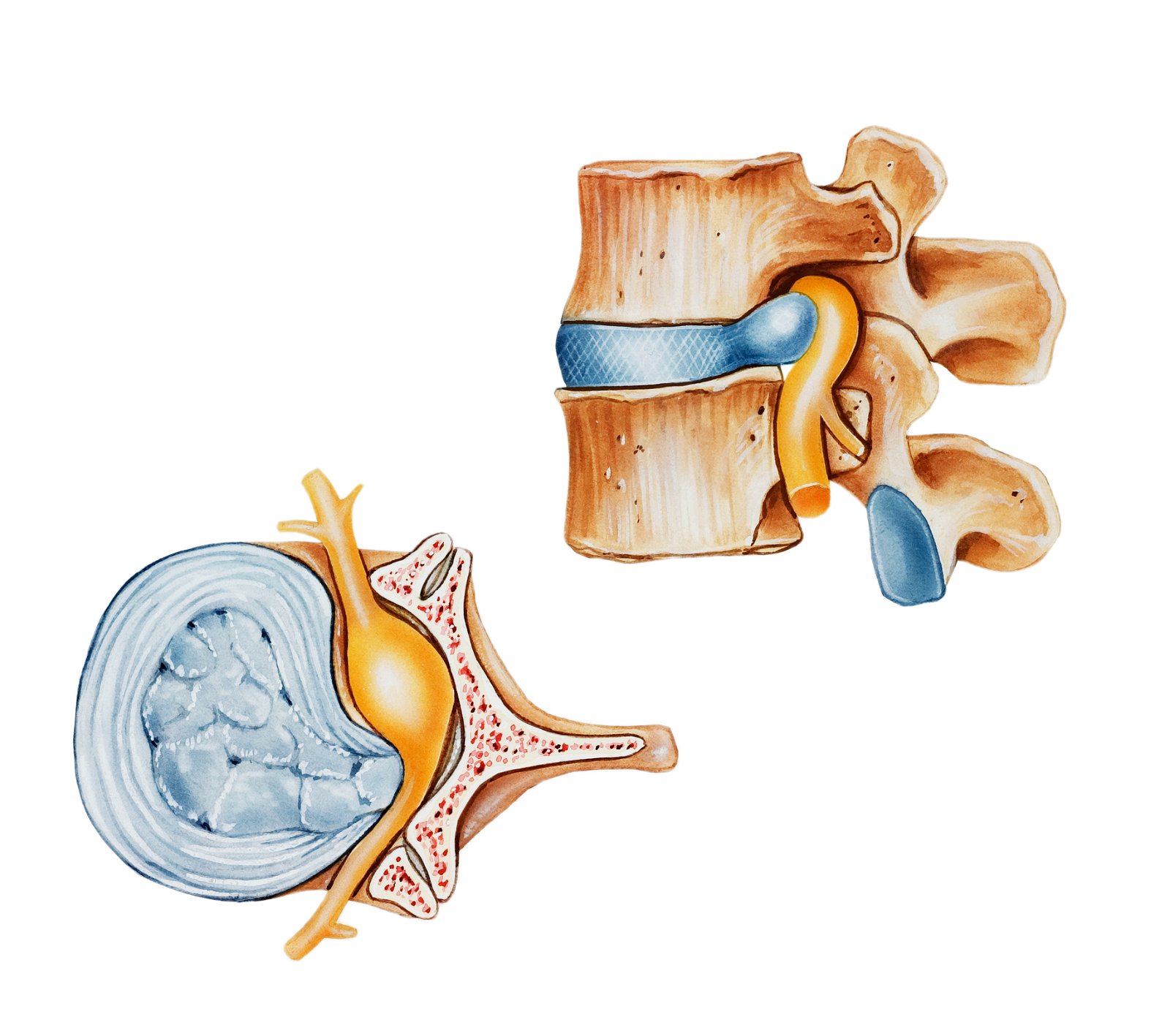
To understand the development of a herniated disc, basic knowledge of the anatomical structure of the spine is necessary. The spine is an anatomical structure that gives shape to our torso. The spine is made up of vertebrae, between which are intervertebral discs.
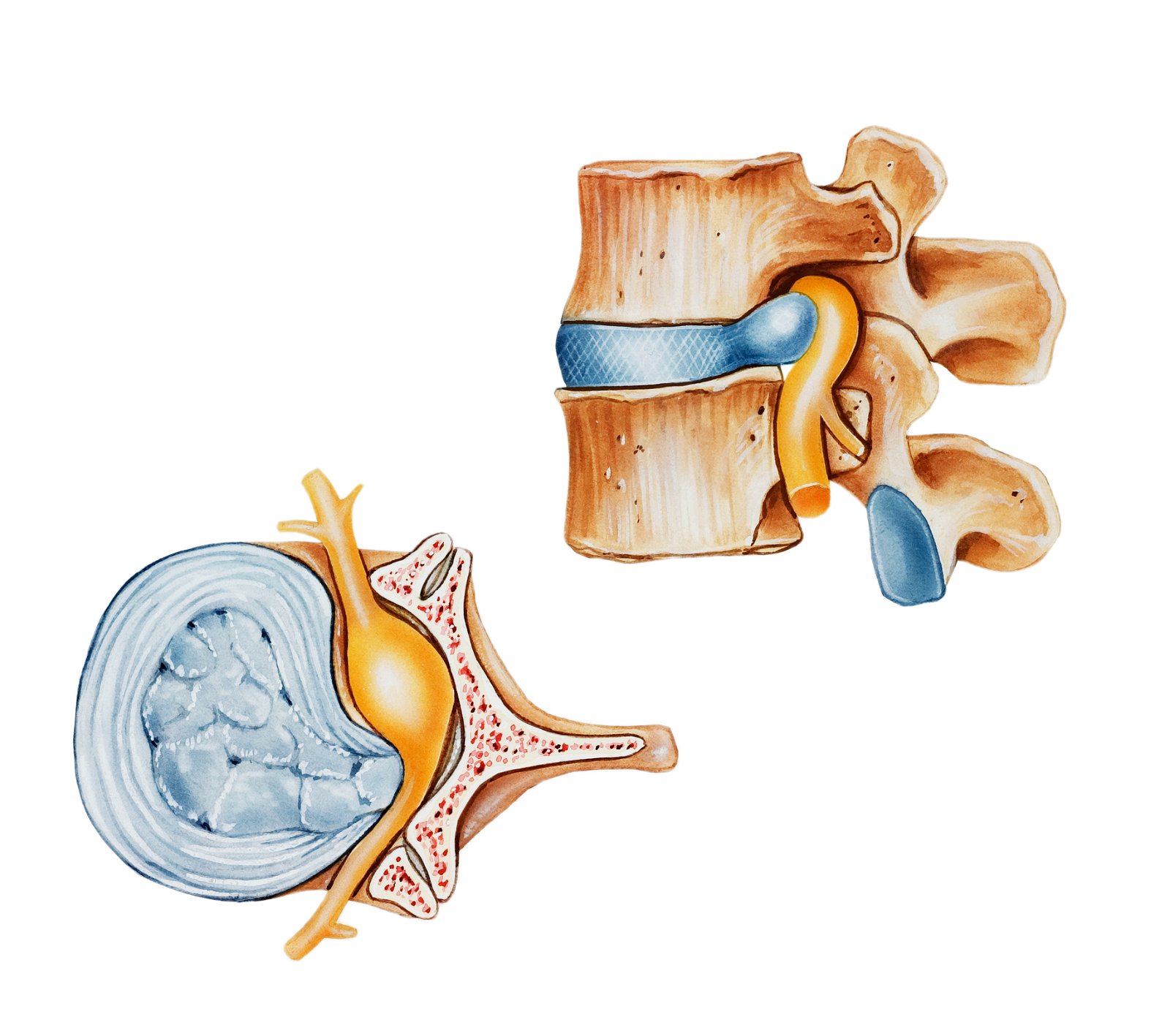
Intervertebral discs are made up of a fibrous ring (annulus fibrosus) and a pulpous core (nucleus pulposus), and their primary function is to absorb vertical forces acting on the spine. The vertebral bodies and vertebral arches enclose the spinal canal in which the spinal cord is located. The vertebrae function as one of the main protective factors of the spinal cord.
Did you know that without intervertebral discs, the spine cannot perform three-dimensional movement? Without the proper “cushions” between the vertebrae, we would not be able to even look over our shoulder.
Causes of a herniated disc
In most cases, a herniated disc occurs due to an inappropriate lifestyle, which leads to repetitive stress and pressure on the intervertebral discs. This category includes a sedentary lifestyle, insufficient movement and physical activity, and above all, physical weakness and improper lifting techniques.
The worst position for the development of a herniated disc (disc herniation) is the bent torso or bent spine position, which is the most common position in most of today’s sedentary occupations. With a constant “flexed” (bent) posture, we develop muscle imbalances, which later manifest themselves during movement and sports activity.
Flexed posture is also dangerous because it reduces disc hydration. Disc hydration is ensured by spinal movement; dehydrated discs are less resistant to forces and offer less protection to the spine.
With constant and inappropriate stress on the intervertebral discs, degenerative changes in the spine gradually occur. Degeneration causes the intervertebral discs to wear down, and the discs can also bulge into the spinal canal, causing its narrowing or spinal stenosis.
The most common causes of herniated discs are:
- Disc degeneration: With age, intervertebral discs can wear out and lose their flexibility and elasticity. This can lead to the formation of cracks in the outer part of the disc.
- Spine injuries: Injuries such as accidents, falls, or lifting heavy loads with improper technique.
- Poor posture: Poor posture, especially when sitting or lifting objects, can create an imbalance in the spine loads and increase the risk of developing a herniated disc. Scoliosis or kyphosis can also affect the development of a herniated disc.
- Genetic predisposition: Certain genetic predispositions may increase the risk of developing a herniated disc, as certain genetic changes in the structure of the disc may increase its susceptibility to injury.
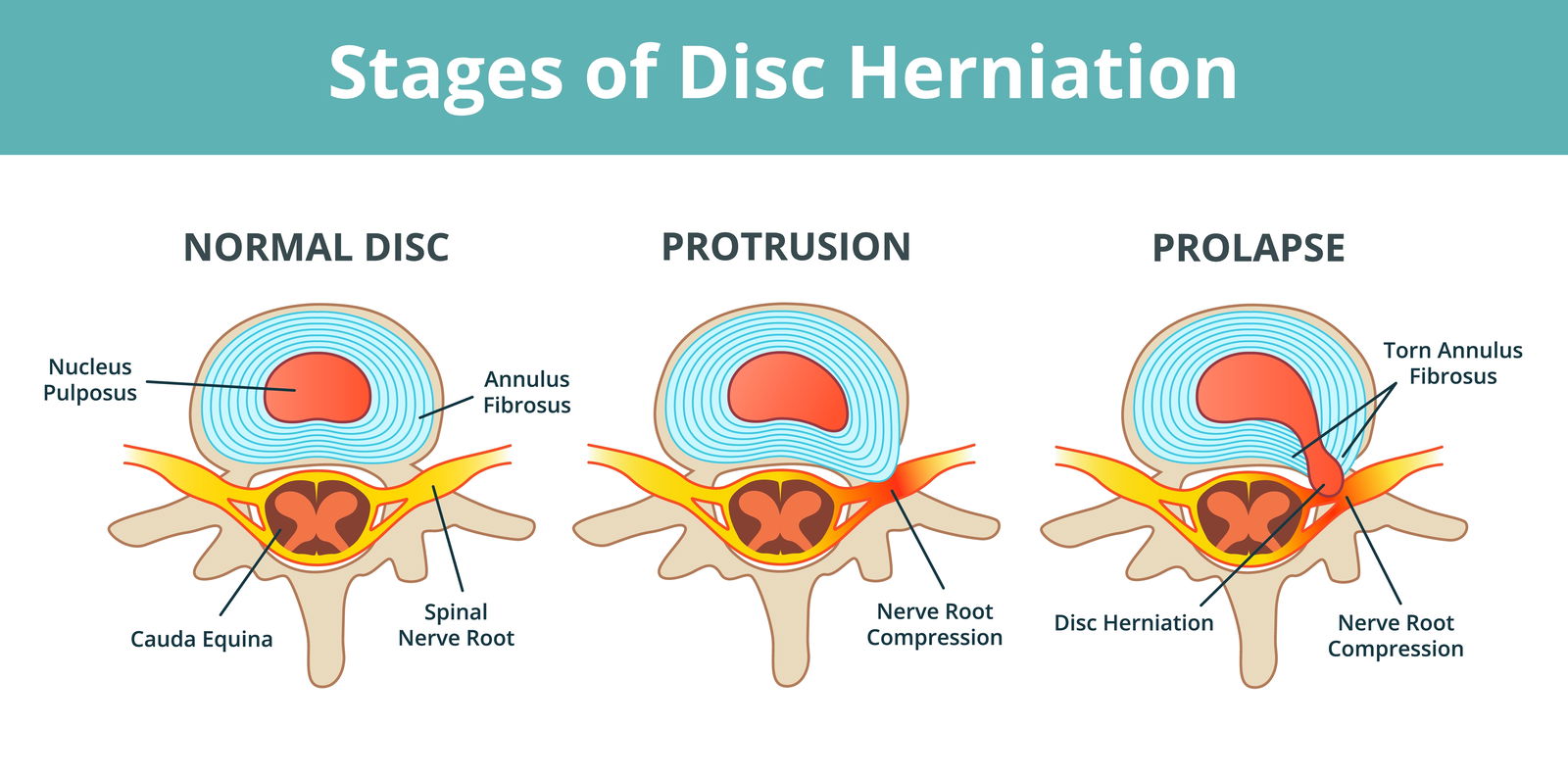
A common pathological change in the intervertebral disc is a rupture or tear of the annulus fibrosus, which leads to leakage of the disc nucleus posteriorly and consequently causes pressure on the spinal canal and compression of the spinal nerves. Pressure on the nerves causes severe pain due to compression, and at the same time, there is chemical irritation of the nerves by the fluid that spills along the nerve roots when the disc ruptures.
DANGERS AND PITFALLS OF DELAYED REHABILITATION

MEDICOFIT specialists
- Delayed rehabilitation causes muscle weakness, which increases the risk of further injuries and serious problems with spinal stability.
- Without proper rehabilitation, you increase your risk of needing surgery, which carries its own risks and complications for mobility.
- Without timely rehabilitation, pressure on the nerve roots can increase, leading to permanent neurological disorders and loss of function.
Inadequate or delayed rehabilitation seriously jeopardises an individual’s long-term physical health and is the main culprit for unsuccessful results and permanent movement limitations.
In most cases, a herniated disc occurs due to an inappropriate lifestyle, which leads to repetitive stress and pressure on the intervertebral discs.
There are several different types of disc herniation. According to the general classification, they can be divided according to the region of the spine where they occur. The most common herniated disc is in the lumbar spine region, but it can also occur in the thoracic spine region (these are rarer – approximately 0.1% to 3% of all herniated discs) and in the cervical spine region, which is the most complex from a rehabilitation perspective; surgical procedures in the area of the seven cervical vertebrae also carry a high risk.
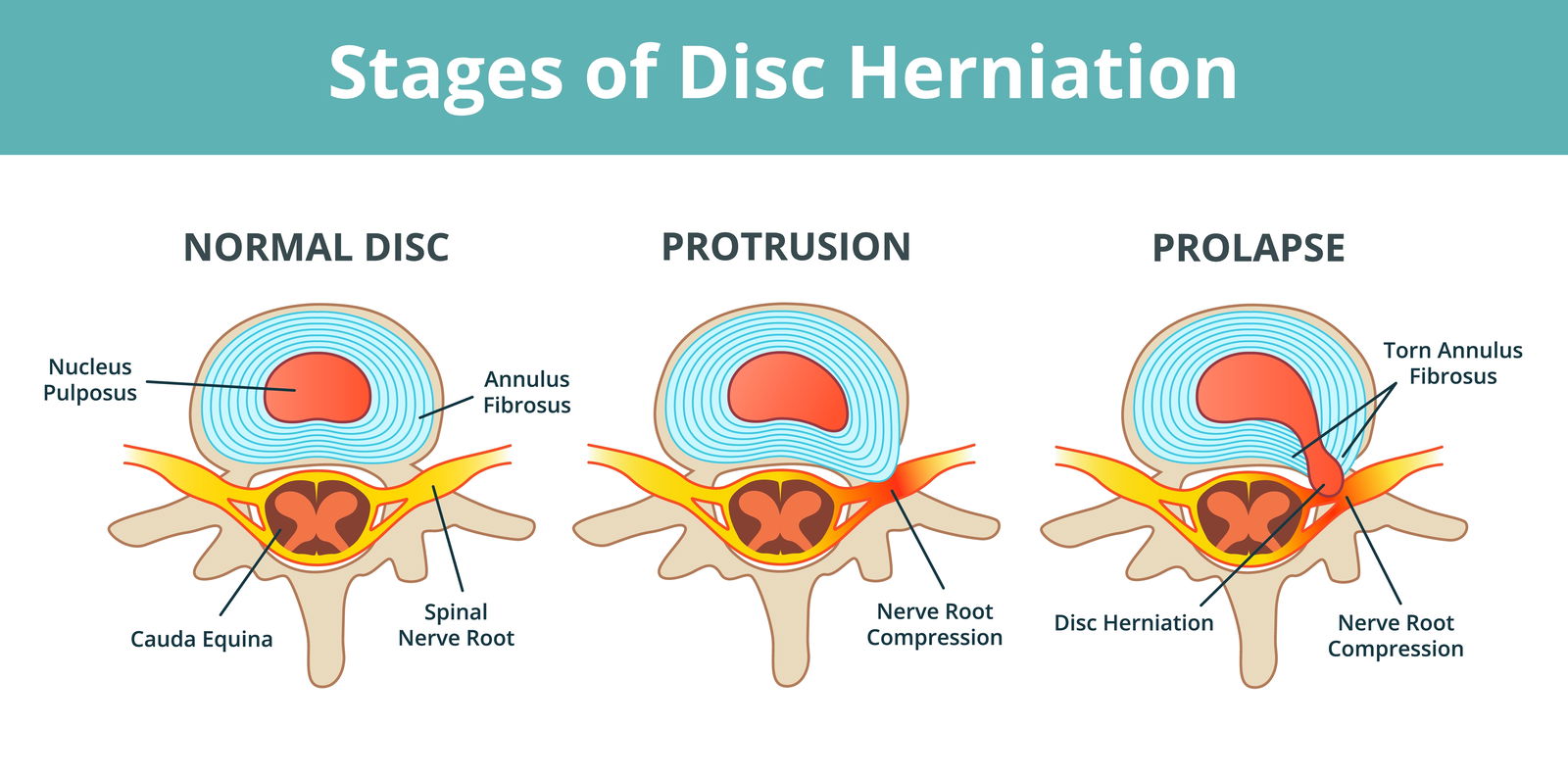
A herniated disc can also be classified based on the degree of degeneration of the intervertebral disc. We distinguish between the following four conditions:
- DISC PROTRUSION (the nucleus of the disc breaks through the annulus without rupturing it)
- DISC EXTRUSION (the annulus is torn, the nucleus slips into the epidural space)
- DISC PROLAPSE (the disc pierces almost the entire annulus, only the outer fibres of the annulus hold it in place)
- DISC SEQUESTRATION (released free fragment that breaks off from the intervertebral disc)
A herniated disc develops gradually; the fibrous ring around the nucleus of the disc does not rupture all at once, as its rupture is the result of a long-term, inappropriate lifestyle.
What symptoms does a herniated disc cause?
The main symptom that accompanies disc herniations (as many as 92% of cases) is pain, which can occur locally in the low back, in a wider area from the low back to the buttocks, or it can radiate down the leg to the level of the toes. Approximately 60% of patients also experience various symptoms of nerve damage, such as movement disorders and loss of muscle strength.
A herniated disc in the lumbar spine often causes compression of the sciatic nerve (so-called “sciatica”), which is the culprit for pain radiating down the leg, often to the foot. A herniated disc can cause a pathological condition called spinal stenosis or narrowing of the spinal canal.
In the long term, spinal stenosis can lead to wear and tear of the so-called “facet” joints of the spine and the development of bone outgrowths on the spine’s processes – spinal osteoarthrosis.
WHEN TO OPT FOR MEDICOFIT DIAGNOSTIC THERAPY?
- Persistent pain in the low back or neck that radiates to the extremities.
- Presence of neurological symptoms such as weakness, numbness, or tingling in the arms or legs.
- If you have previously had problems with pain in your spine and the symptoms are recurring, this means that the injury was not properly treated or that a new injury has occurred.
At MEDICOFIT clinic, we provide patients with scientifically supported specialist physiotherapy for herniated disc, which begins with booking a diagnostic therapy appointment.
When symptoms typical of a herniated disc appear, it is necessary to undergo diagnostic therapy and prepare an individualised rehabilitation training programme. The MEDICOFIT physiotherapy specialist always ensures appropriate patient education, as this is the only way rehabilitation can be successful in the long term.
Book an appointment for herniated disc rehabilitation
How is a herniated disc treated?
Scientific literature and rehabilitation practice in recent years show the exceptional success of conservative rehabilitation of herniated discs compared to surgical treatment. The most effective method for long-term relief from back pain is professional, individualised training.

Back pain is not always an indicator of a degenerated spine, and conversely, we also know that a painless spine does not mean that degeneration is not present. Many patients report successful outcomes from treatment of back pain caused by a herniated disc using training. Herniated disc rehabilitation should be conservative, specifically with training, mobilisation, and anti-inflammatory medications.
Scientific literature and practice in the field of conservative treatment of spinal pain show that herniated disc can be cured in 60% to 90% of patients with an appropriate training approach, so a conservative approach to rehabilitation is an advantage over surgery for most patients.

We also opt for surgery if herniated disc rehabilitation with training has not been successful, but a conservative approach should definitely have priority. Most patients choose to rehabilitate a herniated disc through training, as it is an effective treatment method with a low risk of complications.
Surgical treatment of herniated disc is recommended especially when there are more severe neurological disorders or urinary and faecal incontinence.
When is herniated disc surgery necessary?
The diagnosis of a herniated disc is made by an orthopaedist by evaluating the radiological image or results of a magnetic resonance imaging scan of the patient’s spine. Indications for emergency surgery for herniated disc are extremely rare and do not exceed 5% of all cases diagnosed with the pathological condition of herniated disc. Surgical treatment provides sudden relief from pain, but does not eliminate the cause of the herniated disc. Rehabilitation training to strengthen muscles and correct muscle imbalances target the causes that led to the development of spinal problems.
Some indications for urgent surgery for herniated disc are: loss of foot control (foot drop), cauda equina syndrome, urinary and faecal incontinence. Patients often opt for surgical treatment, despite the good prognosis of rehabilitation with training, because pain relief is much quicker.
WHY CHOOSE SPECIALIST PHYSIOTHERAPY TREATMENT?
- We ensure high treatment success and guarantee long-term health of the spine.
- Up to 95% of our patients do not require spinal surgery!
- We offer state-of-the-art non-invasive treatment methods that provide optimal conditions for complete resolution of a herniated disc, without any surgery.
Comprehensive treatment of herniated disc at MEDICOFIT clinic is recommended by numerous renowned orthopaedic surgery specialists.
At MEDICOFIT clinic, we are noticing that patients are increasingly aware of the fact that surgery is unnecessary in most cases, and that the procedure cannot provide complete relief from their problems.
Specialised physiotherapy rehabilitation for herniated disc
A herniated disc is often associated with a one-time situation where a person experienced a “pinch” in their back; however, this movement was actually just a mechanism that exacerbated a long-standing degeneration of the spine to the point that pressure was exerted on the nerve structures. The causes of severe pain in the case of a herniated disc are usually small asymptomatic disc protrusions that have been present for a long time and have formed and increased as a result of poor core muscle structure and incorrect, forced postures.

The key to treating back pain caused by a herniated disc is to do the exact opposite of what is often advised in practice. A longer period of inactivity and rest further weakens muscle structures and can accelerate the mechanism of herniated disc formation, escalate nerve compression, and consequently increase pain.
If a herniated disc has been diagnosed and is not currently causing pain, it is important to undergo a functional examination of movement patterns and muscles and, if necessary, perform personalised training. Asymptomatic disc herniation can be present for a long time and not cause any problems, but carries an absolute high risk for individuals who spend long periods of time in a sitting position and have weakened core muscles or use the core poorly during physical activities.
-
Stage 1: Developing stability of the lumbar spine and reducing pain in basic positions; this phase is specific to the individual’s pain and is combined with specialised physiotherapy treatments.
-
Stage 2: The goal is to establish optimal mobility and control of the pelvis in various natural and compensatory positions.
-
Stage 3: The goal is to increase muscular endurance of the deep abdominal muscles, lateral abdominal muscles, and strengthen the back muscles with basic strength exercises.
-
Stage 4: The last phase is crucial and integrates the core muscle structure, stability and mobility improvements into complex movement patterns, while also increasing muscle strength and endurance in these patterns.
Modern science and practice in treating pain resulting from herniated intervertebral discs find that the greatest rehabilitation success is achieved through systematically implemented training.

The key for anyone suffering from a herniated disc is to not fall into patterns of kinesiophobia, which literally means the fear of movement. Conservative treatment with training is your best strategy and investment.
Medical professionals should be the number one choice when seeking a diagnosis, with physiotherapy being second on the list, as it effectively reduces pain through therapies. Kinesiotherapy, the four-phase training system for treating the causes, is the final phase of spinal pain treatment, which should last intensively for a period of three to six months, and then be maintained for a longer period with a lower volume in the form of support for your lifestyle.
Patient education is key in the rehabilitation process for a herniated disc, and should also include learning the correct lifting technique. Inappropriate lifting technique increases pressure on the intervertebral discs, and can also lead to a host of associated problems and back pain. It is necessary to learn appropriate pressure in the abdominal cavity, which serves as the main protective mechanism for the lumbar spine during movement and lifting loads. Finally, patient education should also include promotion of an active lifestyle (encouraging sufficient activity with the addition of strength and mobility training) and reviewing possible ergonomic adaptations in the workplace.
At MEDICOFIT clinic, we offer effective and professionally supported rehabilitation treatment for herniated intervertebral discs and related pain and problems. Rehabilitation for herniated discs is designed on an individual level of the patient, and the goal is to eliminate pain and also change lifestyle in the long term.
Common surgical procedures for herniated disc
Evacuation of herniated disc (microdiscectomy)
Microdiscectomy is the most common surgery performed on the lumbar spine. During the procedure, a piece of the intervertebral disc that is pressing on the nerve root is removed. The annulus remains intact during the procedure, with the exception of a small entry opening, and allows for good preservation of the height of the intervertebral space. A microsurgical technique is used, so collateral damage to spine-adjacent tissues is minimal.
Lumbar spine decompression
This is a more complex surgical procedure that is used to remove the causes of spinal canal narrowing (spinal stenosis). Several spinal structures can be removed, such as the lamina, ligamentum flavum, spinous processes, part of the facet joints, and osteophytes. The goal of the procedure is to relieve pressure on the nerve roots. The procedure causes collateral damage to the multifidus muscle and consequently acute weakening of the lumbar spine extensors. It is important to note that the scar tissue forms after the procedure, which increases the stiffness of the lumbar spine after the procedure.
Lumbar spine fixation (spondylodesis or spinal fusion)
During the procedure, the spine is stabilised at the primary level (bone grows between two vertebrae) using synthetic implants (screws, rods, cages, artificial bone, etc.). The complete process of fusion of two vertebrae can take several years, ending when the space between the vertebrae has completely ossified. With this procedure, there is an option of delaying certain rehabilitation milestones (walking down the hallway, stairs).
Anterior lumbar interbody fusion (ALIF)
ALIF is a surgical procedure that improves posture and relieves spinal pain by fusing the vertebrae at the lumbosacral junction through an anterior approach. The procedure improves the balance of the spine and reduces the load on the lower back. The procedure is classified as a minimally invasive surgical procedure due to the low rate of collateral soft tissue damage and faster postoperative recovery.
Some data on surgical procedures for herniated discs in the lumbar spine – the average operation time is 75 minutes with fairly low blood loss (49.5 ml), so transfusion is only necessary in around 2% of cases. In 95% of patients, there are no immediate complications during surgery, and 4% of patients repeat the surgery within one year. Approximately 2,800 surgeries for herniated intervertebral discs are performed in Slovenia annually, and according to scientific literature, more than half of them are unnecessary, as the condition could be improved with training rehabilitation.
Exercises for rehabilitation of herniated disc
Some effective exercises for the rehabilitation of a herniated disc include trunk stabilisation exercises, which are based on trunk extension, learning appropriate pressure in the abdominal cavity, and general trunk stabilisation. It is also crucial to perform anti-rotational exercises and semi-dynamic exercises in plank positions.
In the image, you can see exercises for the spine that you can do in the comfort of your own home. We recommend that all patients contact a physiotherapist in case of persistent pain, as they may otherwise perform home exercises incorrectly and cause more harm than good.
Herniated disc surgery removes the acute symptoms, but not the cause. To prevent recurrence of problems, physiotherapy rehabilitation of the herniated disc is necessary.
Book an appointment for herniated disc rehabilitation
Chiu, C. C., Chuang, T. Y., Chang, K. H., … in Hsu, W. Y. (2015). The probability of spontaneous regression of lumbar herniated disc: a systematic review. Clinical Rehabilitation, 29(2):184-195.
Court, C., Mansour, E. in Bouthors, C. (2017). Thoracic disc herniation: surgical treatment. Orthopaedics and Traumatology: Surgery and Research, 104:531-540.
Earhart, J. S., Roberts, D., Roc, G., … in Wellington, H. (2012). Effects of lumbar disk herniation on the careers of professional baseball players. Orthopedics, 35:43-49.
Hayden, J. A., van Tulder, M. W. in Tomlinson, G. (2005). Systematic review: strategies for using exercise therapy to improve outcomes in chronic low back pain. Annals of internal medicine, 142(9), 776–785.
Heliövaara, M., Mäkelä, M., Knekt, P., Impivaara, O. in Aromaa, A. (1991). Determinants of sciatica and low-back pain. Spine, 16(6), 608–614.
Koes, B. W., van Tulder, M. W. in Peul, W. C. (2007). Diagnosis and treatment of sciatica. BMJ, 334:1313-1317.
Quint, U., Bordon, G., Preissl, I., … in Rosenthal, D. (2012). Thoracoscopic treatment for single level symptomatic thoracic disc herniation: a prospective followed cohort study in a group of 167 consecutive cases. European Spine Journal, 21:637-645.
Sakou, T., Masuda, A., Yone, K. in Nakagawa, M. (1993). Percutaneous discectomy in athletes. Spine (Phila Pa 1976), 18:2218-2221.
Videman, T., Nurminen, M. in Troup, J. D. G. (1990). Lumbar spinal pathology in cadaveric material in relation to history of back pain, occupation and physical loading. Spine, 15(8):728.
Weinstein, J. N., Tosteson, T. D., Lurie, J. D., … in Deyo, R. A. (2006). Surgical vs nonoperative treatment for lumbar disk herniation: the Spine Patient Outcomes Research Trial (SPORT): a randomized trial. JAMA, 296(20), 2441–2450.
Yamaguchi, J. T. in Hsu, W. K. (2019). Intervertebral disc herniation in elite athletes. International Orthopaedics, 43(4):833-840.