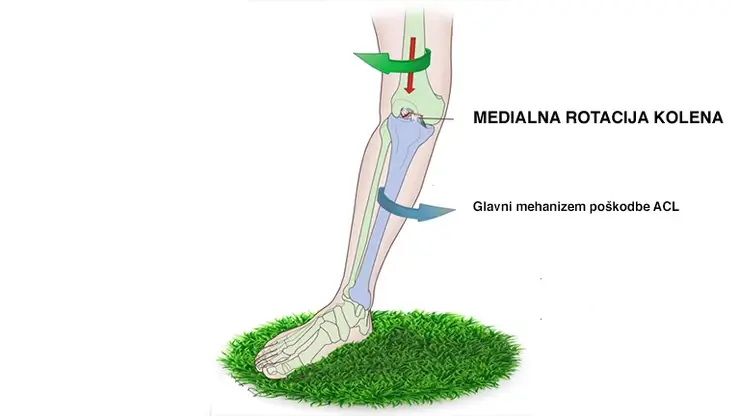
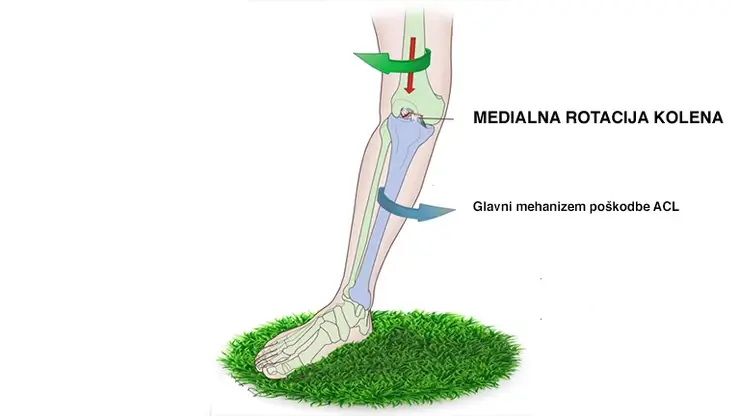
In general, there are two mechanisms of anterior cruciate ligament injury, a non-contact mechanism and a contact mechanism of injury.
70-80% of anterior cruciate ligament injuries are non-contact in, meaning that the cause of the injury is not an external force such as an onslaught, blow or fall. A non-contact injury is caused by ligament failure.
A large number of injuries can therefore be prevented by adequate physical preparation for sporting activities, which means choosing intelligent movement programs and diagnostics.
ACL contact injury
A common way of injury in team sports is a blow or impact to the knee from the side in a position of hyperextension or internal rotation of the knee (often in football).
In martial arts where elements of grappling are involved, the knee is typically forced into positions of internal rotation or hyperextension on which levers, transitions or weight transfers are then applied, leading to ligament damage.
Non-contact injury to the ACL
Often occurs in ball sports in the following situations:
- After landing on one outstretched leg.
- After landing on one leg and simultaneously turning quickly inwards or outwards after landing.
- When turning quickly inwards or outwards on one leg while the foot is fixed and not turned in the direction of the player’s pivot (common in basketball and handball).
- When stopping quickly with one step on the outstretched leg (often in basketball).
- Long step to the side and internal rotation of the knee on the other leg (often in volleyball).
- Landing on both feet and inward rotation of both knees (often in volleyball).
- Landing on both feet with insufficient flexion of the knees and hips (common in volleyball).In alpine skiing, the anterior cruciate ligament is the most commonly injured ligament in the knee, and the injury occurs:
- Due to the ski being pulled backwards and sideways when the skier gets into the valgus position of the knee.
- When the skis are suddenly pulled forward and inwards and the weight is suddenly shifted backwards.
- Landing too deeply after a jump when the skier transfers too much weight backwards
The injured person often hears a blow (pok) in the knee. This is characterized by a feeling of instability of the knee, which occurs immediately after the injury and may later temporarily disappear due to increased swelling. The pain usually increases for 1 week, then gradually decreases.
Typically, the leg cannot be burdened immediately after the injury. A protective spasm occurs, which is characteristic of all knee injuries and causes limited mobility of the knee joint in flexion and extension. The protective spasm typically lasts for 4 weeks, is more intense for the first 14 days, and persists as long as the knee is unstable.
The injury is most characterized by the following signs:
– Severe pain in the knee.
– Restricted knee mobility (knee extension and flexion).
– Edema or swelling that occurs several hours after the injury and gradually increases.
– Pain may radiate to the whole limb.
– Possible bleeding under the skin.
– Feeling of instability of the knee, feeling of swaying, floating of the knee.
– Gradual loss of muscle mass of the quadriceps femoris, especially in the inner part.
”The function of the anterior cruciate ligament is to control the forward displacement of the tibia, when the ACL is injured, the forward displacement of the tibia relative to the femur is increased, resulting in impaired medial rotation and knee instability.”
”Often after an injury, when the ligament is completely or partially torn, we have the feeling that our knee is giving out or that our knee is floating, and some patients also describe the feeling of an empty knee. The main function of our ligaments is to keep the intra-articular movements within safe amplitudes or to keep our joint strong.”
”Any injury to the ligaments, therefore, means potentially greater intra-articular movements and less stability of the knee. The sensation of the knee buckling and floating means that we feel greater intra-articular movements that are not natural and interfere with normal joint mechanics.”
”In addition to ligaments, muscles are also responsible for the stability of our joints and are the secondary stabilizers of the knee. The stability of a joint that has a damaged ligament will depend primarily on the training of our muscles”.
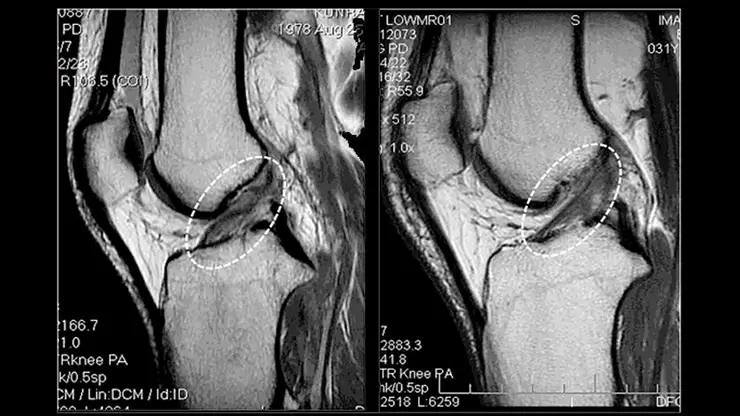
The injury is confirmed with clinical tests carried out by a physiotherapist (Lachman test, Anterior Compartment test, Lelli test) and by magnetic resonance imaging (MRI), which confirms the suspicion of an ACL injury and potential damage to other joint structures.
Diagnosis is often hampered in the initial phase if MRI tests are not performed immediately after the injury before swelling develops, otherwise, the swelling must first be reduced, which hinders an accurate diagnosis. It is advisable to perform an MRI as soon as possible after the suspected injury, as the accuracy of clinical tests to assess the anterior cruciate ligament in the early phase after an injury is questionable due to various limiting factors such as swelling, pain, and fear of the injured person.
Magnetic resonance imaging is the most reliable and appropriate method for the diagnosis of injuries suggestive of an anterior cruciate ligament. Physiotherapy diagnosis with the above anterior cruciate ligament tests compares the difference in forwarding displacement of the tibia between the two limbs. Magnetic resonance imaging provides an accurate assessment of the inside of the knee, typically damaging not only the cruciate ligament but also other structures such as the meniscus, cartilage, medial or lateral collateral ligaments, etc.
It is important to know that there is no single diagnostic method that can give a true functional assessment of the joint with 100% accuracy and determine the appropriate treatment, so it is recommended to perform several tests simultaneously to decide on the treatment.
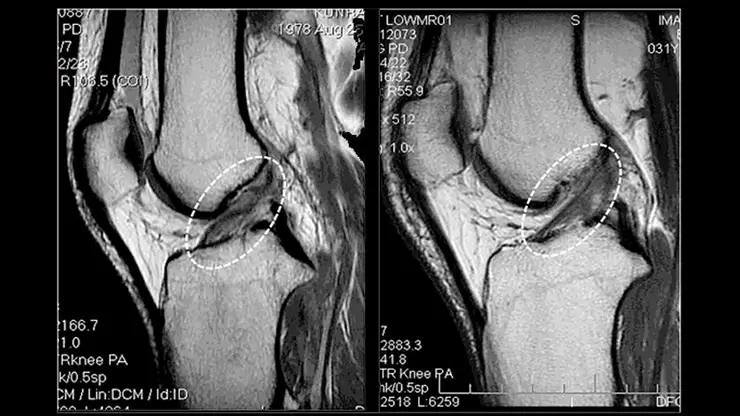
Damaged ACL levo and healty ACL desno
Treatment is generally divided into conservative and operative (ACL reconstruction).
Conservative
Conservative treatment is primarily used by the elderly and the inactive. People who have only minimal strain in their daily activities and have severe pain and instability of the knee do not need surgical treatment.
However, if surgery is not an option, appropriate ‘management’ of the joint with specific exercises to keep the muscles involved toned and the symmetry between them properly maintained is necessary.
Operative – ACL reconstruction
In the case of surgical ACL reconstruction, it is essential that the kinesiologist or physiotherapist, the physician and the injured person agree on a pre-operative exercise plan and also decide on plans for continuing sporting activities after surgery and the corresponding post-operative exercise.
Main types of cruciate ligament reconstruction
- Anterior cruciate ligament reconstruction from the graft of the tendon muscles and the adductors semitendinosus and gracilis
The advantages are a smaller incision and slightly less pain. The disadvantage is the slower ingrowth of tendons into the bone, which results in a longer rehabilitation period. The operation also significantly reduces the muscular strength of the posterior loci, i.e. the power of contraction of the knee joint.
- Anterior cruciate ligament reconstruction with patellar bone tendon (BTB)
This method is the gold standard, with excellent and highly predictable results. The main disadvantages are that the graft removal requires a larger incision at the front of the knee, which means an aesthetic deformity. Pain is intense in the early post-operative period, there is a greater chance of patellar tendinitis after surgery, slower recovery of knee extension strength, and greater atrophy of the anterior thigh muscle.
- Reconstruction of the anterior cruciate ligament with the quadriceps tendon
The quadriceps tendon is the ligament above the kneecap, and the incision can be made with or without the bony part. The advantage of this graft compared to a patellar ligament graft is the lower likelihood of chronic inflammation and pain. Another advantage is that the osseous part of the graft can be bone grafted in the canal.
- Anterior cruciate ligament reconstruction from posterior lodge fibres using the double bundle technique (the latest technique)
Anatomical double bundle ACL reconstruction ensures that the cruciate forces are applied more reliably and allows better control of knee movement in the anterioposterior direction and in rotation. The most commonly used technique is single-bundle anterior cruciate ligament reconstruction (methods 1,2,3). In this case, however, the anteromedial and posterolateral anterior cruciate ligament bundles are reconstructed separately. In this way, the normal anatomy of the anterior cruciate ligament is restored and the rotational stability of the knee is improved.
”In most cases, a knee joint without a cruciate ligament is unstable to the extent that any sporting activity poses a risk. A knee joint without a cruciate ligament is in most cases unstable, leading to various anomalies of the knee joint during movement.”
”The most common consequence of a torn cruciate ligament is twisting or buckling of the knee during sporting activity, walking down stairs and during everyday activities. Often it is a feeling that we have to be extremely careful with the knee or the joint will give way.”
”A patient with a torn cruciate ligament can function normally without surgery by eliminating potentially risky sporting activities, but has a higher risk of damage to other knee structures such as the meniscus and cartilage, and in the long term osteoarthritis may occur. Without the cruciate ligament, the knee wears out and is damaged more quickly by twisting and knee bending in the absence of regular specialised exercise, resulting in micro instability leading to increased intra-articular movements and overloading of the remaining structures. ”
”Surgery is often advised for younger people and those who are active in sport.”
ACL injuries are a rare injury in children but unfortunately become more common in the teenage years as a result of overuse or poor fitness. In the case of a partial rupture, there is a potential for regeneration, and conservative treatment and a short phase of immobilisation of the joint are usually sufficient. However, if a complete rupture with a positive Lachman test and instability of the joint is detected, surgical treatment of the ligament, which is rarely performed before the age of 10 years, is indicated.
Stages of knee healing after an anterior cruciate ligament injury
Exercise is a key part of successful anterior cruciate ligament reconstruction. Exercises should be started immediately after surgery and pre-operative exercise is recommended. After surgery, the knee is cooled with ice. The knee should be progressively stretched and muscle strength should be strengthened, and above all, full knee extension should be achieved as soon as possible.
Consistency in treatment is important, as is a serious approach on the part of the patient undergoing the operation and very strict adherence to the instructions of the orthopaedic surgeon, physiotherapist and kinesiologist. In practice, patients often discontinue treatment before ACL rehabilitation is complete, which poses a significantly higher risk of re-injury.
In principle, mobilisation with the support of crutches and gradual loading of the operated leg to the point of pain starts on the first post-operative day. Most patients use crutches for up to three weeks.
With new surgical techniques and new graft fixation techniques, it is possible to use an accelerated treatment protocol. Nevertheless, rehabilitation is complete when the graft is firmly embedded in the bone. This is usually five to seven months after surgery, depending on the type of graft used and the course of rehabilitation.
The old classification divided the rehabilitation of the anterior cruciate ligament into 3 phases (an extremely ill-defined exercise system which in practice poses a higher risk of re-injury of the ligament), whereas the modern classification considers 6 phases of rehabilitation, of which the first phase is pre-operative, the second is focused on the management of the acute post-operative condition, and the remaining weight is borne by the specialised training or the rehabilitation of the anterior cruciate ligament.
TOTAL REHABILITATION LASTS 6 – 9 MONTHS CONTINUED BY THE SYSTEMATIC MODEL OF PROGRESSIVE REHABILITATION OF THE KNEE JOINT.
Discontinuation of treatment before the end of the 6th month means proven increased complications and the possibility of re-injury of the ligaments. For the first 6 months, rehabilitation is specific and is carried out by a qualified physiotherapist or kinesiologist. If there are complications, there is a possibility of prolonging the rehabilitation.
Phases of rehabilitation
PHASES OF REHABILITATION OF THE FRONT CIRCULAR CONNECTION – method of operative treatment:
- PRE-OPERATIVE PHASE (8 – 0 weeks before the operation).
- FIRST POST-OPERATIVE PHASE (0 – 3 weeks)
- SECOND PHASE POST-OPERATIVE (4 – 6 weeks)
- THIRD PHASE POST-OPERATIVE (7 weeks – 3 to 4 months)
- FOURTH PHASE POST-OPERATIVE (4 – 6 months)
- FIFTH PHASE POST-OPERATIVE (6 to 9 – 12 months)
“All phases are defined according to the type of surgery, i.e. the choice of the graft, the damage to the remaining structures, the age of the patient and the type of sports activities. Healing and ligamentisation of the graft after surgery are widely studied areas and define the exact system of exercises in each phase of rehabilitation”.
** PRE-OPERATIVE PHASE
After an acute anterior cruciate ligament injury, regardless of the treatment modality, it is important to use physiotherapy to reduce traumatic oedema, normalise mobility and strengthen muscles and proprioception. In order to improve rehabilitation, physiotherapy is recommended before surgery.
The aim of pre-operative treatment is to:
- Build up strength and muscle mass, which in practice means that the absolute atrophy (loss of muscle mass) after surgery will be less and, consequently, rehabilitation will be quicker.
- To increase nerve innervation before surgery, which means that muscle activation will be much faster after surgery
- To familiarise the patient with the treatment methods and to accurately assess the functional capacity of the muscles and joints, which serves as a basis for the design of a post-operative rehabilitation plan
The pre-operative phase is mandatory for all athletes and a very wise investment for all other injured people. As the level of physical fitness increases, the likelihood of re-injuring the knee decreases inversely.
- HEALING PHASE OF FRONT ACL INJURY (0-3 weeks)
**For the first 6 weeks, knee flexion must not be forced beyond a 90 degree angle!
Objectives:
- To gain 90 degrees of knee flexion range of motion.
- To gain full knee extension.
- To independently activate the anterior thigh muscle.
- Walk without crutches by the end of the second week.
Phase goals and limitations may vary depending on concomitant damage to the remaining structures in the knee joint.
- HEALING PHASE FOR FRONT ACL INJURY (3-6 weeks)
In the second phase, specific strength exercises are performed to establish basic control of the knee joint.
Objectives:
- To gain 120 degrees of knee flexion.
- Natural walking pattern without limping.
- Normal stair gait with good knee control.
- Improvement of muscular endurance and proprioception.
- HEALING PHASE OF FRONT CIRCULATOR INJURY (6 weeks – 3 to 4 months)
Increase intensity of strength exercises, patient may also perform lateral dynamic exercises and isokinetic strength exercises. Athletes can start with lower intensity exercises on the coordination ladder and preparation for plyometrics. Athletes can start with the technical basics of the sport.
Objectives:
- To increase the patient’s confidence in his/her knee.
- Progressive increase in strength of the knee muscles and transition to the basics of plyometrics and running.
- One body weight eccentric lowering on one leg to the right angle or in a push-up apparatus for athletes and non-athletes.
- Olympic bar squat to right angle – half the added body weight on the bar for athletes.
- Achieves 85% bilateral symmetry in isolated knee extension and flexion strength.
- HEALING PHASE OF FRONT CIRCULAR BUCKLE INJURY (4 – 6 months)
In the fourth phase, the aim is to reach the maximum strength capacity needed for the client to return to his/her regular activities. This phase will vary considerably from athlete to recreational or to the physically inactive individual. The aim is to master normal running speed and the basics of plyometrics such as jumps, push-ups and push-ups for all athletes. For all non-active athletes, the aim of Phase 4 is to reach peak endurance in strength and maximal power. At the end of Phase 4, most of the inactive athletes will have reached the status of completed rehabilitation.
- The athlete must have reached all the strength criteria for his/her sport (depending on the specifics of each sport).
- All movements are performed without full range of motion compensations.
- At the end of the phase, all athletes who are not active in the sport reach the status of completed rehabilitation of the anterior cruciate ligament in the absence of other complications.
- At the end of the phase, the athlete can return to sports training, but only in low to medium intensity non-contact training forms, work on technical elements is recommended.
- Normal running speed is achieved.
- Jumping, rebounding and accelerating or stopping no longer cause pain.
- HEALING PHASE FOR FRONT CIRCUS INJURY (6 to 9 – 12 months)
Phase 5 is reserved for athletes and all those who are not active in sport, who have had complications with previous phases or who have delayed or stopped rehabilitation by their own choice.
For all those who are not active in sport, the aim is to reach the criteria of the previous phases insofar as they have not been achieved.
- Athletes perform demanding plyometric exercises.
- Athletes develop maximal strength.
- Athletes make the transition to standard conditioning.
- Athletes gradually return to the full intensity of standard training.
- Athletes may return to competition after the completion of the phase, provided that all phases have been performed systematically without interruption or complications.
- Athletes shall be granted the status of completed rehabilitation after the completion of the phase, provided that there are no complications.
Anterior cruciate ligament rehabilitation is one of the more complex processes in modern physiotherapy and kinesiology. At its core, it is about the patient’s gradual adaptation to the load he/she carries in the normal rhythm of life and adherence to the rules of graft ligamentization. The exercise process must be planned, carried out without interruption and monitored by diagnostics.
The main contemporary problem is the search for self-care on social platforms and the self-healing of the injury. The likelihood of an anterior cruciate ligament rupture recurring within the first two years after surgery is 6x higher. One in four athletes tears the anterior cruciate ligament of the other, non-injured leg within 24 months after anterior cruciate ligament reconstruction on the injured leg. 9 – 12% of all patients who undergo anterior cruciate ligament reconstruction re-rupture the ligament. Among patients under 18 years of age, 31% re-rupture the anterior cruciate ligament, i.e. one in three juvenile athletes can expect to undergo reconstruction again.
I have cited the above facts as a reminder of the need for professional and systematic work in the postoperative or conservative management of the injured anterior cruciate ligament. The level of physical fitness that a patient needs to achieve to move safely after ACL reconstruction or return to sport is often underestimated.
PHASES OF REHABILITATION OF THE FRONT CIRCULAR BAND – method of surgical treatment
Conservative treatment is used with patients who do not opt for surgery or are not suitable candidates for surgery. Adults who are not active in sports or the elderly should first start with conservative treatment of the anterior cruciate ligament if there is no damage to the supporting structures in the knee joint.
The standards to be achieved by the patient in conservative treatment are the same as the standards of post-operative rehabilitation for all individuals who are not active in sport. In the first weeks after the injury, swelling is reduced and therapeutic techniques are used to alleviate pain in the joint. Gradually, the range of movement is increased and the joint is progressively loaded with basic strength exercises.
A joint without a cruciate ligament or with a partially torn ligament functions normally with basic movements and strength exercises, but care should be taken when performing accelerated and rotational movements and contact activities should be avoided.
If anterior cruciate ligament surgery is not an option, it is essential to have continuous management of the knee with exercise, as increased muscle strength will increase active stabilization of the joint and have a “shielding” effect.