This website uses cookies so that we can provide you with the best user experience possible. Cookie information is stored in your browser and performs functions such as recognising you when you return to our website and helping our team to understand which sections of the website you find most interesting and useful.
The knee joint is considered one of the most complex joints within the human body and presents with a high incidence of injury. Due to its anatomical structure and high exposure to external forces, it is one of the most commonly injured joints. A knee sprain is regarded as a traumatic injury and not as a degenerative process of the knee ligaments. Trauma usually occurs when a high force impact causes an overextension of the fibres of the soft knee tissues, which usually results in pain, swelling and hematoma.
The most common type of ligament damage is the rupture of the ACL (anterior cruciate ligament) and/or the MCL (medial collateral ligament) (International Journal of Physical Education, Sports and Health 2020).
On a yearly basis 80.000 to 250.000 cases of injury to the anterior cruciate ligament (hereinafter ACL) occur. Approximately 80% of ACL ruptures are of non-contact etiology due to uncontrolled forces (i.e. due to a sudden shift in direction). The incidence of damage to the medial collateral ligament (hereinafter MCL) accounts for 7,9% of all (sports related) injuries.

An increased incidence of injury can be observed in physically active individuals (Logerstedt et al., 2017). A knee sprain can lead to a rupture of any of the knee ligaments, although this is not always the case. Following a knee sprain it is essential to carry out diagnostic procedures in order to accurately assess the severity of the anatomical and functional damage.
The anatomical structure of the knee joint
The knee joint is an articulation of the femur, patella and tibia bone. The articular surfaces of the femur and tibia bone are incongruent, so compatibility of the two surfaces is provided by two fibrocartilaginous structures – the medial and lateral meniscus. Due to their elasticity the two meniscuses are resistant to contact forces. A majority of the forces are being transmitted to the meniscuses, which thanks to their elasticity protect the articular cartilage from injuries.
The meniscus basically acts as a shock absorber, as it protects the articular cartilage. The elastic tissue of the meniscus ensures that the forces which are transmitted to the femur and tibia bone are buffered. Thus, a more optimal distribution of the synovial fluid within the joint can be achieved.
What actually is the anterior cruciate ligament (ACL)?
Ligaments are structures connecting two bones. The knee has four main ligaments that surround the joint, two of which are located on the inside of the joint and cross each other; these are the anterior and posterior cruciate ligament. The other two major ones are the medial and lateral collateral ligament. Together, the anterior (ACL) and posterior cruciate ligament (PCL) form a structure within the knee, increasing its stability and allowing dynamic movement of the joint.
The ACL extends from the posterolateral part of the tibia and attaches to the lateral aspect of the femur. It is comprised of strong fibrous fibers and is, according to statistics, the most frequently injured of the four knee ligaments. The ACL provides 85% of the restraining force to anterior tibial displacement and medial tibial rotation.
After ACL reconstruction, effective pain treatment along with appropriate strengthening of the knee structures is of key significance. Both can be achieved by increasing the stability and range of motion of the knee joint during the postoperative phase. In principle the reconstructed ligament connects the intercondylar notch of the tibia to the medial aspect of the lateral femoral condyle.
Due to its essential role in the stabilization of the knee joint it restricts the anterior displacement of the tibia and thus prevents the hyperextension of the knee, which is characteristic in individuals with ligamentous laxity. Literature states that the ACL is divided into two bundles, namely into the anteromedial (AM) and posterolateral (PL) bundle.
Knee sprain grades
Knee sprains are divided into 3 grades according to their level of severity, with the grade 1 indicating only a stretched or mildly torn ligament. The knee is usually painful and swollen. Grade 2 indicates a partial tear of the ligament, accompanied by more profuse swelling, bleeding into the affected joint, hematoma and increased pain, which makes it impossible to put weight on the injured leg. The range of motion of the knee is compromised as well.

A grade 3 injury involves a complete tear of the ligament, leading to knee instability. Such an injury requires surgical treatment, as the ligaments do not have the ability heal properly on their own.
The most prevalent symptoms after such an injury include:
- Cracking or popping when bending the knee,
- Pain that is often sharp and stabbing and can be felt in the area of the patella,
- Inability to lift heavy objects,
- Swelling,
- Fluid buildup behind the patella,
- Knee instability.
Treatment
Treatment of a knee sprain can be carried out operatively (reconstruction) or conservatively. An interdisciplinary approach is necessary in order to determine if an operative procedure is the only remaining treatment option. Individuals who opt for reconstructive surgery have to be aware of the length of the rehabilitation process. ACL reconstruction surgery can be performed with four types of grafts: with the tendon of the gracilis and semitendinosus muscle, with the patellar tendon, the quadriceps tendon, or the hamstring graft method.
Whether or not to opt for an operative procedure is decided by a doctor, based on the damage to the knee ligaments.
Diagnostics after a knee sprain:
The condition can be evaluated with different clinical diagnostic tests:
- Pivot shift test: internal tibial rotation can be performed to asses an ACL tear and decrease in the knees range of motion.
- Lachman test: performed by pulling on the tibia in order to assess an ACL rupture.
- Anterior drawer test: with the knee bent at a 90⁰ angle, the tibia is moved anteriorly and posteriorly. Excessive displacement of the tibia anteriorly suggests an ACL injury, whereas excessive posterior displacement of the tibia may indicate damage to the PCL. (Arundale et al. 2021).
When tension in the knee appears, ligament damage should be evaluated first (International Journal of Physical Education, Sports and Health 2020). Any type of knee injury, as in our case a knee sprain, should be acutely treated following the RICE principle, which is applicable within the first 72 hours after the injury has occurred.


RICE
R- rest; Immediately following the injury you should cease the physical activity, as it can make the situation even worse and prolong the overall treatment process.
I-ice; Start cooling the affected area as soon as possible. Cold compressions (cryopak, icepack), massaging with ice or immersion of the affected area into ice water reduces swelling and relieves pain.
C-compression; pressure or compression: bandaging of the injured body part prevents additional accumulation of fluid (swelling). The bandage must not be too tight as it can impede blood flow. Cold compressions can be applied on top of the bandage.
E-elevation; elevation of the affected limb above the level of the heart allows the blood and lymph to flow towards the heart. As a result, swelling and pain can be reduced. This way gravitation can aid in reducing swelling. Particular caution should be taken in individuals with congestive heart failure.
When does the rehabilitation process start?
The rehabilitation process should be started immediately after the acute phase, which means as soon as an improvement cannot be achieved by measures you take at home. The rehabilitation process is started gradually, with stretching of the unloaded knee and until pain is felt. Later the injured lower limb can be cyclically loaded with the full bodyweight.
Considering the fact that rehabilitation of joint injuries and injuries to the surrounding tissues usually takes 6 weeks, an appropriate rehabilitation structure has to be determined.
What does research regarding knee sprains suggest?
Research suggests that proprioceptive training is a key component in the rehabilitation process following knee injuries, as this type of training strengthens both the bodies ligament and receptor system. The predominant receptors, required for this type issues are receptors capable of detecting the joint position and movement.
Special knee exercises following a knee injury
Proprioceptive training helps with strengthening of the neuromuscular connection and thus allows for improved dynamical stability of the joint. Reduced coordination and lack of balance on the other hand prolong the time necessary to achieve the previous level of mobility. Adequate proprioception allows the proprioceptive reflexes to regulate muscle activity and movement (the so-called intermuscular coordination), improving movement execution.
Exercises targeted at improving proprioception include closed kinetic chain exercises along with any type of exercise that enhances balance (example: standing on the balance board with one leg and catching & throwing a ball). Strength training is primarily used to strengthen the knee flexor muscles, hip abductors and core stabilizer muscles (Gidu and Oltean, 2016).
Physiotherapy following a knee sprain
The rehabilitation plan targeted at the accelerated injury healing can include the use of various physiotherapeutic methods, such as TECAR (Trasderimento Energetico Capacitivo e Resistivo) or LASER (Light amplification by stimulated emission of radiation) therapy.
High-quality electrostimulation can promote the activity of specific slow (type 1) or fast twitch (type 2) muscle fibers, which mimics the activation that occurs during loading of the muscles. When paired with coordination exercises it has also been shown to have an important impact on the increase in eccentric muscle strength.
TECAR therapy is a beneficial non-invasive thermo therapy which allows the transmission of energy deep towards the center of the injury. It relieves pain and promotes lymph and venous drainage. It reduces tendon and bursa inflammation, soft tissue pain and helps with joint, bone and muscle injuries (Yeste – Fabregat, 2021).
Laser therapy is a medical treatment method which promotes the metabolic and healing process of the damaged tissue as the penetrating light has biological and physiological effects. The therapy improves nerve conduction and stimulates the healing of the affected tissue (wound, bedsore, ulcer etc.) (Farivar et al., 2014).
In terms of injury prevention, a lot can be done simply by choosing the right footwear, with proper stretching and muscle strengthening exercises, which help to stabilize the knee joint.

Returning to physical activity after a knee sprain
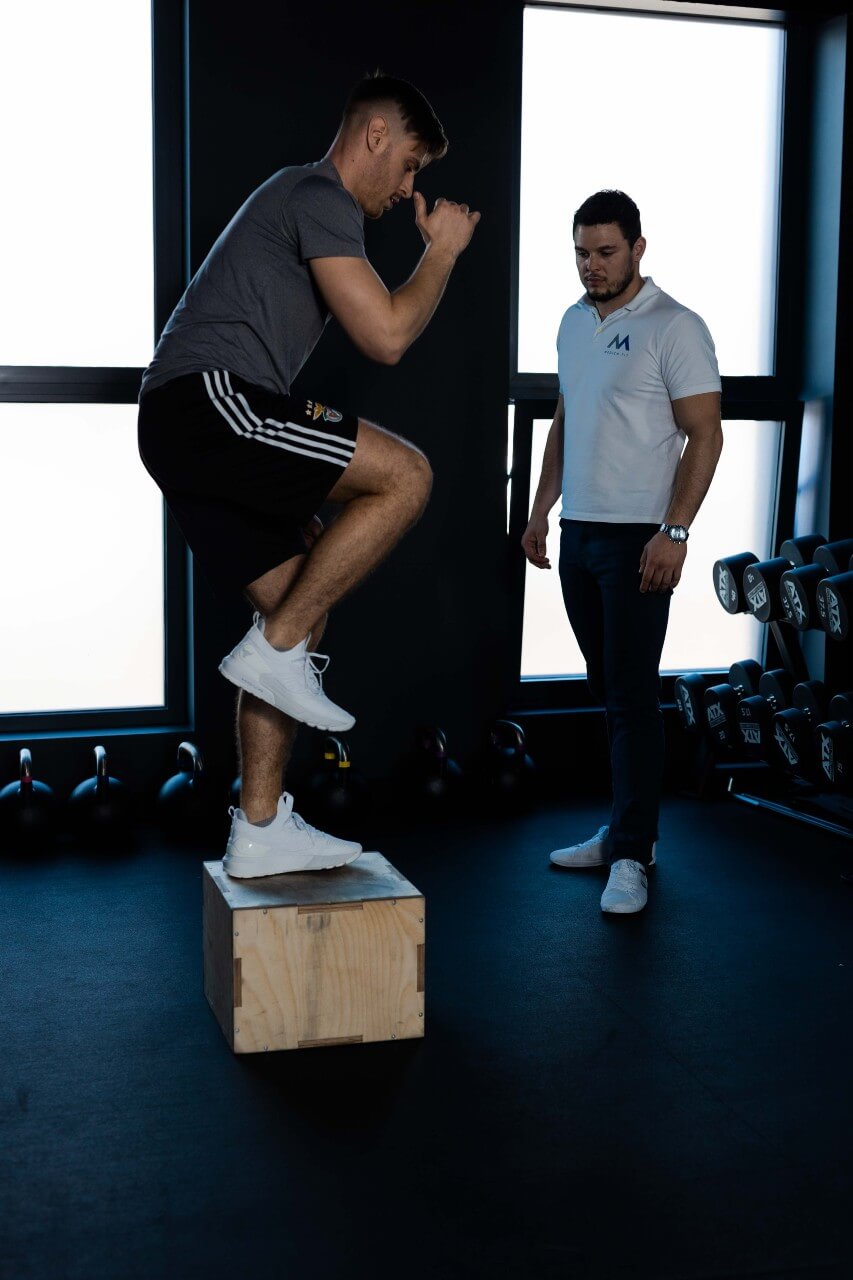
The average time it takes to return to physical activity following a knee injury is 3 to 4 weeks. Individuals should return to the training process (at least in the beginning) under the watchful eye of qualified professionals, who are going to monitor the progress and inform the athletes about the post-injury mechanism of the ligaments and surrounding structures.
Exercises which include jumping, balance pattern movements, flexibility and the gradual incorporation of external forces into the training regime, are the result of a positive treatment outcome following a knee injury.
Strong muscles are a key component which ensures the effective stabilization of the knee joint and reduces the risk for damage of the passive knee stabilizers (ligaments, meniscuses), such as an ACL injury due to a knee sprain (Mehl et al, 2017).
At Medicofit we combine injury rehabilitation with physical preparation. Along with the treatment of injuries we also focus on improving your physical performance and the prevention of possible injuries. We remain by your side during your rehabilitation process and help you achieve optimal physical preparation.

References
- International Journal of Physical Education, Sports and Health, 2020. Rehabilitation of knee injuries in Kabaddi players of Punjab. Dostopno na: https://www.kheljournal.com/archives/?year=2020&vol=7&issue=1&part=B&ArticleId=1619.
- Logerstedt, David S., David Scalzitti, May Arna Risberg, Lars Engebretsen, Kate E. Webster, Julian Feller, Lynn Snyder – Mackler, Michael J. Axe in Christine M. Mcdonough. 2017. Knee Stability and Movement Coordination Impairments: Knee Ligament Sprain Revision 2017. Dostopno na: https://pubmed.ncbi.nlm.nih.gov/29089004/.
- Markatos, K., M. K. Kaseta, S. N. Lallos, D. S. Korres in N. Efstathopoulos. 2013. The anatomy of the ACL and its importance in ACL reconstruction. Dostopno na: https://link.springer.com/article/10.1007%2Fs00590-012-1079-8#citeas.
- Gidu, Diana Victoria in Antoanela Oltean. 2016. Benefits of the proprioceptive training in recovery after knee sprain – theoretical grounds. Dostopno na: https://web.a.ebscohost.com/abstract?site=ehost&scope=site&jrnl=2285777X&AN=113336552&h=V6Kxr1v2pizJTQrTVLgQpZy%2bAOzOsoT1OI60KInG9qXMZDIIT4JciUHXW4S3cTzTrUFsvvDY23ZUaaeJQVJ%2bug%3d%3d&crl=c&resultLocal=ErrCrlNoResults&resultNs=Ehost&crlhashurl=login.aspx%3fdirect%3dtrue%26profile%3dehost%26scope%3dsite%26authtype%3dcrawler%26jrnl%3d2285777X%26AN%3d113336552.
- Arundale, Amelia J. H., Mario Bizzini, Airelle Giordano, Timothy E. Hewett, David S. Logerstedt, Bert Mandelbaum, David A. Scalzitti, Holly Silvers-Granelli in Lynn Snyder-Mackler. 2021. Exercise -Based Knee and Anterior Cruciate Ligament Injury Prevention. Dostopno na: https://pubmed.ncbi.nlm.nih.gov/30170521/.
- Mehl, Julian, Theresa Diermeier, Elmar Herbst, Andreas B. Imhoff, Thomas Stoffels, Thore Zantop, Wolf Petersen in Andrea Achtnich. 2017. Evidence-based concepts for prevention of knee and ACL injuries. 2017 guidelines of the ligament committee of the German Knee Society (DKG). Dostopno na: https://link.springer.com/article/10.1007/s00402-017-2809-5#citeas.
- Farivar, Shirin, Talieh Malekshahabi in Reza Shiari. 2014. Biological effects of low laser therapy. Dostopno na: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4291815/.
- Yeste – Fabregat, Mireia, Luis Baraja – Vegas, Juan Vicente – Mampel, Marcelino Perez – Bermejo, Iker J. Bautista Gonzalez in Carlos Barrios. 2021. Acute Effects of Tecar Therapy on Skin Temparature, Ankle Mobility and Hyperalgesia in Myiofascial Pain Syndrome in Professional Basketball Players: A Pilot Study. Dostopno na: https://www.mdpi.com/1660-4601/18/16/8756.









